COPD Maintenance: How Triple Inhaler Therapy Reduces Exacerbations
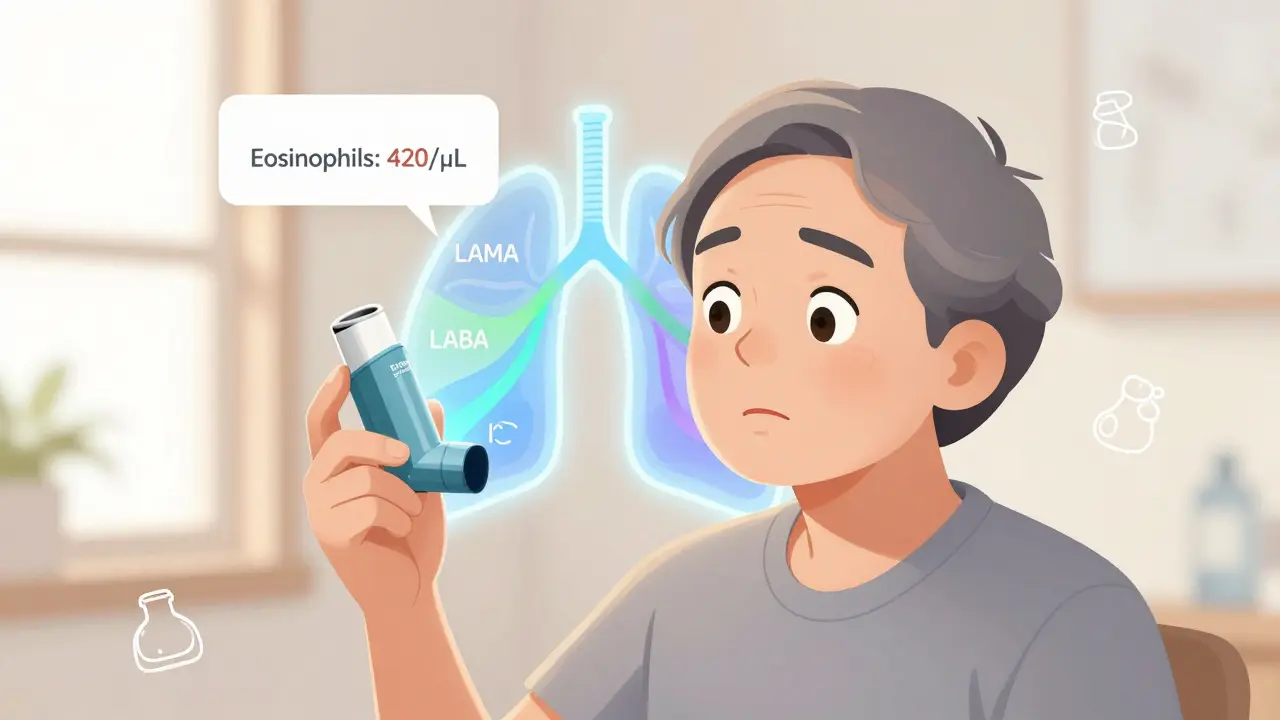
For people with moderate to severe COPD who keep having flare-ups, the goal isn’t just to manage symptoms-it’s to stop hospital visits before they happen. One of the most talked-about tools in COPD maintenance today is triple inhaler therapy. It combines three medications in one device: a long-acting muscarinic antagonist (LAMA), a long-acting beta-agonist (LABA), and an inhaled corticosteroid (ICS). Together, they tackle airway narrowing, inflammation, and mucus buildup all at once. But it’s not for everyone. The key is knowing who benefits-and who could be harmed.
Who Actually Needs Triple Therapy?
Not every COPD patient needs three drugs. The 2024 GOLD guidelines make this clear: triple therapy is only recommended for those who’ve had two or more moderate flare-ups in the past year, or one severe flare-up that landed them in the hospital. And even then, it’s not automatic. Your blood eosinophil count must be 300 cells/µL or higher. This number acts like a biological signal-it tells doctors your airways are inflamed in a way that responds to steroids.If your eosinophil count is below 100, triple therapy offers little to no benefit. In fact, it increases your risk of pneumonia without helping your breathing. That’s why doctors now test this count before prescribing. It’s not just a routine blood test-it’s a decision-maker.
Single Inhaler vs. Multiple Devices
There are two ways to get triple therapy: either three separate inhalers (multiple-inhaler triple therapy, or MITT) or one device that delivers all three (single-inhaler triple therapy, or SITT). The difference isn’t just convenience-it’s survival.Real-world data from the TARGET study shows 78.4% of patients stuck with SITT after 12 months. For MITT? Only 62.1%. Why? People forget. They get confused. Carrying three inhalers around is a hassle. One study found that 42.7% of patients on multiple devices simply forgot doses. Another 29.3% didn’t know which one to use when.
When patients switched from MITT to SITT, their exacerbations dropped by 37% in just six months. The reason? Simplicity. One puff, once a day. No mixing up devices. No missed doses. Devices like Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol) and Trimbow (budesonide/glycopyrronium/formoterol) are designed for ease. But they’re not interchangeable.
How the Medications Work Together
Each component has a job:- LAMA (like umeclidinium or glycopyrronium) relaxes the muscles around your airways, keeping them open.
- LABA (like vilanterol or formoterol) does the same thing but works faster and lasts longer than older bronchodilators.
- ICS (like fluticasone or budesonide) reduces the chronic inflammation that makes your lungs more sensitive to triggers like cold air or smoke.
Used together, they don’t just add up-they multiply. A 2018 NEJM study showed that in patients with eosinophil counts above 300, triple therapy cut moderate-to-severe flare-ups by about 25% compared to dual bronchodilators. But that benefit faded after 90 days in some trials, suggesting the biggest win comes early.
Extrafine particle formulations-like those in Trimbow-penetrate deeper into the lungs, meaning lower doses can be just as effective. That’s why some doctors prefer budesonide-based regimens: they’re just as good at reducing exacerbations but carry a lower pneumonia risk than fluticasone.

The Pneumonia Risk You Can’t Ignore
Steroids suppress inflammation-but they also weaken your lungs’ natural defenses. That’s why pneumonia is the biggest danger with triple therapy. Studies show patients on fluticasone-based triple inhalers have a 1.83 times higher risk of pneumonia than those on budesonide.The FDA requires a black box warning for all ICS-containing inhalers. The EMA says you must review your need for steroids every 3-6 months. If your eosinophil count drops below 100, or if you haven’t had a flare-up in a year, it’s time to reconsider. Many patients stay on triple therapy far longer than they should-not because it’s helping, but because no one checked.
Why Some Experts Say It’s Overused
There’s a growing debate. Dr. John Blakey from the University of Western Australia argues that many trials showing triple therapy’s benefits were flawed. In the IMPACT and ETHOS trials, nearly 40% of patients were already on triple therapy when they enrolled. When they were switched to dual therapy (LAMA/LABA), their flare-ups spiked-not because dual therapy was weak, but because they were abruptly pulled off steroids.Real-world data from a UK study of 31,000 COPD patients found no difference in first exacerbation risk between SITT and LAMA/LABA when you account for this withdrawal effect. That means the “magic” of triple therapy might be partly an artifact of stopping steroids too quickly.
Professor Jadwiga Wedzicha, who led the IMPACT trial, still stands by the results for high-eosinophil patients. But she agrees: “It’s not a one-size-fits-all.” The consensus now? Use it only when the biomarker says yes.

Cost, Access, and Real-Life Struggles
In the U.S., brand-name triple inhalers like Trelegy Ellipta can cost $75-$150 a month out-of-pocket. For Medicare beneficiaries, that’s a barrier. A 2022 study found 22.3% skipped doses because they couldn’t afford it. That’s not non-compliance-it’s survival.Some patients get generic alternatives, but options are limited. In Australia, PBS subsidies help, but not everyone qualifies. Clinics in Perth are seeing more patients switching to dual therapy when they can’t pay, even if their eosinophil count is high. That’s a dangerous compromise.
Adherence isn’t just about remembering to take your inhaler. It’s about understanding how to use it. Ellipta devices require specific breathing techniques-inhale deeply, hold for 5 seconds, then exhale slowly. A 2022 study found it takes 7.2 minutes to teach proper technique, compared to 4.8 minutes for standard inhalers. If you don’t get the technique right, the medicine doesn’t reach your lungs. That’s why 50-70% of “treatment failures” are actually just bad inhaler use.
What Comes Next?
The future of COPD care is personal. Researchers are testing new biomarkers like fractional exhaled nitric oxide (FeNO) to predict steroid response better than eosinophils alone. In phase 3 trials, biologics like dupilumab are showing promise for patients with high eosinophils, offering an alternative to steroids.By 2027, experts predict most advanced COPD patients will be guided by blood or breath tests-not just symptoms. Triple therapy won’t disappear. But its role will shrink. It’ll be reserved for those who truly need it: frequent exacerbators with high eosinophils, good inhaler technique, and the means to afford it.
For now, if you’re on triple therapy, ask your doctor: Why am I on this? Is my eosinophil count still high? Have I had a flare-up in the last year? Could I try stepping down? Your lungs don’t need more drugs-they need the right ones, at the right time.
Who qualifies for triple inhaler therapy in COPD?
Triple therapy is recommended for adults with moderate to severe COPD who have had two or more moderate exacerbations, or one severe exacerbation requiring hospitalization in the past year-and whose blood eosinophil count is 300 cells/µL or higher. It’s not for everyone. If your count is below 100, the risks (like pneumonia) outweigh the benefits.
Is single-inhaler triple therapy better than using three separate inhalers?
Yes, for most people. Single-inhaler triple therapy (SITT) improves adherence by 15-20% compared to multiple-inhaler regimens. Patients report fewer missed doses, less confusion, and simpler routines. Real-world data shows switching from multiple inhalers to one device reduces exacerbations by 37% in six months. The convenience directly translates to better outcomes.
Does triple therapy reduce COPD mortality?
No. Neither the FDA nor the European Medicines Agency found evidence that triple therapy lowers death rates. The benefit is in reducing flare-ups, not extending life. The focus should be on preventing hospital visits and improving daily function-not on false hopes about survival.
What’s the biggest risk of using triple inhaler therapy?
Pneumonia. Inhaled corticosteroids suppress lung defenses, making infections more likely. Fluticasone-based regimens carry a 1.83 times higher risk than budesonide-based ones. Anyone on triple therapy should watch for fever, increased mucus, or worsening cough-and get checked immediately if symptoms appear.
Can I stop using my triple inhaler if I feel better?
Don’t stop without talking to your doctor. Feeling better doesn’t mean the inflammation is gone. If your eosinophil count drops below 100 or you haven’t had a flare-up in a year, your doctor may suggest stepping down to a dual bronchodilator. Stopping suddenly can trigger a flare-up. Always reassess every 3-6 months.
How do I know if I’m using my inhaler correctly?
Many people think they’re using their inhaler right-but they’re not. Studies show 50-70% of treatment failures are due to poor technique. Ask your doctor or pharmacist to watch you use it. Use a checklist: shake it, breathe out fully, seal lips, inhale slowly and deeply, hold breath for 5 seconds, then exhale. For Ellipta devices, you must inhale hard and fast. If you’re unsure, get a refresher every six months.

Shelby Marcel
January 26, 2026 AT 04:45i just got prescribed trelegy and honestly thought it was gonna be a miracle drug but then i read about the pneumonia risk and now i’m terrified lmao
Alexandra Enns
January 26, 2026 AT 05:03Oh please. You think this is new? I’ve been telling my doctor for years that steroids are just a band-aid. Canada’s been pushing dual therapy for years and we’re not drowning in ER visits. This triple therapy hype is Big Pharma’s latest cash grab. Eosinophils? Please. My cousin’s count was 280 and he’s been fine on LAMA/LABA for 3 years. Stop overmedicating people.
And don’t even get me started on the cost. $150 a month? In Canada we get it subsidized, but in the US? You’re literally choosing between breathing and eating. This isn’t medicine-it’s exploitation.
Also, the whole ‘one puff a day’ thing? That’s a lie. I’ve watched patients fumble with Ellipta for 20 minutes. If you don’t inhale hard enough, the medicine hits your tongue and you taste it. That’s not adherence-that’s failure disguised as convenience.
And why do we always ignore the fact that most COPD patients smoke? No amount of inhalers fixes a habit that’s literally burning your lungs. Fix the root cause before throwing steroids at the problem.
And don’t even get me started on the ‘black box warning’ being buried in the pamphlet. You think patients read that? No. They see ‘three drugs in one’ and think ‘wow, this is advanced.’ It’s not advanced-it’s dangerous.
I’ve seen people on this stuff get pneumonia twice in a year. And then they blame the cold weather. No. It’s the fluticasone. The FDA knows it. The EMA knows it. But the reps still hand out free samples like candy.
And don’t tell me ‘it’s for high eosinophils.’ My neighbor’s was 350 and she’s been in the hospital 4 times since starting it. Biomarkers aren’t magic. They’re suggestions. Doctors need to think, not just follow guidelines.
Triple therapy isn’t the future. It’s a dead end. We need biologics. We need better diagnostics. We need to stop pretending that more drugs = better outcomes.
Also, why is no one talking about the fact that most of these studies are funded by the same companies that make the inhalers? Conflict of interest much?
And yes, I’ve read the IMPACT trial. And yes, I know Jadwiga Wedzicha’s name. But her data included people already on triple therapy. Of course they crashed when pulled off. That’s not evidence-it’s a rebound effect.
Stop glorifying this. It’s not a breakthrough. It’s a gamble with your lungs.
Marie-Pier D.
January 27, 2026 AT 00:42Hey, I just wanted to say I totally get where you’re coming from, Alexandra 😊
My mom’s on Trelegy and honestly, we were scared too-but she’s had zero flare-ups for 14 months now, and her eosinophil count is still at 410.
She’s also had pneumonia training from her pulmonary nurse-like, real step-by-step videos and a checklist. It made all the difference.
And yes, the cost is insane… but her pharmacy has a patient assistance program. I know it’s not perfect, but for some of us, it’s working.
Just please, don’t write it off completely. It’s not magic, but for the right person? It’s life-changing. 💙
Chloe Hadland
January 27, 2026 AT 05:40I’ve been on LAMA/LABA for 5 years and honestly? I feel better than I did on triple therapy. I had one mild flare-up last year, but I didn’t end up in the hospital. My doctor said my eosinophils dropped below 100 so we switched. Best decision ever. No more fungal throat infections. Just… peace.
Amelia Williams
January 28, 2026 AT 21:04Okay I just read this whole thing and I’m crying. Not because I’m sad, but because this is the first time I’ve seen someone explain COPD like it’s not just ‘bad lungs’ but like… a whole system. The part about inhaler technique? I thought I was doing it right for 3 years. Turns out I was just puffing like a cigarette. 7 minutes to teach it? That’s insane. My clinic does it in 2 and then says ‘you got it.’
Also-biologics? I’ve been begging my doctor to test me for dupilumab. I have high eosinophils but I’m terrified of steroids. If there’s a non-steroid option, I’m all in. Can someone link the trial info??
Sawyer Vitela
January 29, 2026 AT 19:50Triple therapy doesn’t reduce mortality. End of story. Stop pretending it does. You’re not saving lives-you’re delaying hospital visits. Big difference.
asa MNG
January 31, 2026 AT 17:41bro i just got my first triple inhaler and i’m already addicted to the way it feels 😭 i mean it’s like my lungs finally chill the f*** out but now i’m scared to stop because what if i go back to wheezing like a broken accordion??
also why does my doctor keep asking me about my eosinophils like i’m a science experiment??
and why is this thing so expensive?? i’m on medicaid and they said ‘try the generic’ but there isn’t one??
also i think i’m using it wrong but i’m too embarrassed to ask again 😅
Karen Conlin
January 31, 2026 AT 23:33Let me tell you something that no one says out loud: the real reason triple therapy works isn’t because of the drugs-it’s because it forces people to stick to a routine. One device. One time a day. No confusion. That’s the magic. The meds are just the vehicle.
And yes, pneumonia risk? Real. But so is the risk of dying from a flare-up you didn’t prevent.
My patient, Maria, went from 4 ER visits a year to zero after switching to SITT. She’s 72, speaks Spanish, and never read a single pamphlet. But she remembers her one inhaler. That’s the win.
Don’t dismiss it because it’s not perfect. It’s not about the science alone-it’s about what works in real life. And for thousands? It’s working.
Also-cost is a crisis. But so is lack of education. If we invested as much in teaching inhaler technique as we do in pushing new drugs, we’d cut exacerbations by 50% without spending a dime.
And yes, we need biologics. We need FeNO. We need better biomarkers. But those won’t be ready for 5 years. Until then? We do what works. With eyes open.
Phil Maxwell
February 1, 2026 AT 10:52Interesting read. I’ve been on dual therapy for 8 years and never had a hospital stay. My eosinophils are usually around 150. I guess I’m just lucky? Or maybe my lungs are just… chill?
Shanta Blank
February 3, 2026 AT 08:47Y’ALL. I JUST GOT OFF TRIPLE THERAPY. AND IT WAS LIKE MY LUNGS WERE WEARING A TIGHT SWEATER FOR 3 YEARS AND SUDDENLY I WAS IN A T-SHIRT AT THE BEACH.
My doctor said my eosinophils dropped to 80. I was terrified to stop. But guess what? I didn’t crash. I didn’t collapse. I didn’t turn into a wheezing ghost.
I just… breathed. Like a normal human.
And now I’m telling everyone: if you feel good and haven’t had a flare-up in a year-ASK TO STEP DOWN. Don’t wait for your doctor to bring it up. You are not your inhaler. You are not your blood count. You are your body. Listen to it.
Also-why is no one talking about how the puffing technique is basically a magic spell? You have to inhale like you’re trying to suck a milkshake through a straw while holding your breath and not coughing. It’s not intuitive. It’s a ritual. And if you mess it up? The medicine just sits on your tongue like a sad little pill.
And yes, I cried when I stopped. Not because I was scared. Because I realized I’d been letting a device define my health for so long.