Switching Between Generic Medications: What You Need to Know

Every time you pick up your prescription, you might get a different pill. Same name. Same dose. But a different color, shape, or imprint. That’s not a mistake - it’s generic drug switching. And it’s happening more than you think.
Over 90% of prescriptions filled in the U.S. are for generic drugs. That’s not because brand names disappeared - it’s because pharmacies and insurers are pushing the cheapest option available. If your levothyroxine was made by Mylan last month and Teva this month, you’re not alone. Millions of people switch between generic manufacturers every year without even realizing it.
Why Do Generic Switches Happen?
It’s simple: money. Generic drugs cost 80% to 85% less than brand-name versions. For insurers, that’s a huge savings. For pharmacies, it’s about filling orders with the lowest-cost supplier. When a patent expires, multiple companies rush to make the same drug. One might sell for $5 a month. Another for $3. The pharmacy picks the $3 one. Next month, the $3 supplier runs out. The pharmacy switches to the $2.50 version. No doctor’s note. No patient warning. Just a different pill in your bottle.
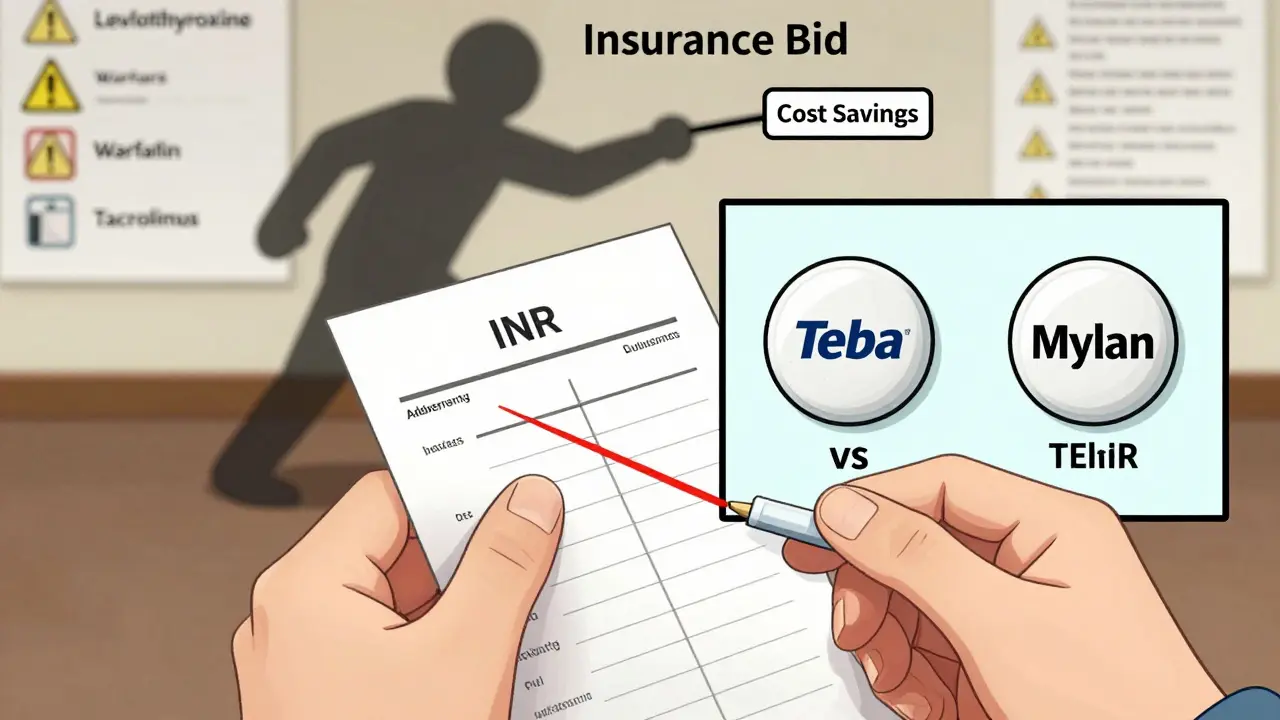
Insurance companies often force these switches. They have contracts with specific generic manufacturers and change them frequently based on bids. Pharmacists are required to dispense the lowest-cost option unless the doctor writes "dispense as written" - and even then, some insurers still override it.
Not All Generics Are Created Equal
The FDA says generics must be "bioequivalent" to the brand-name drug. That means they deliver between 80% and 125% of the active ingredient compared to the original. Sounds close, right? But here’s the catch: two different generics can be at opposite ends of that range. One delivers 80%. Another delivers 125%. That’s a 45% difference in how much medicine your body actually gets.
For most drugs - like statins or blood pressure pills - that variation doesn’t matter. Your body adjusts. But for drugs with a narrow therapeutic index (NTI), even tiny changes can cause serious problems.
When Switching Can Be Dangerous
NTI drugs have a tiny window between being effective and being toxic. A small drop in blood levels? The drug stops working. A small spike? You risk overdose. These include:
- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Tacrolimus (used after organ transplants)
- Phenytoin and other antiepileptics
Patients on levothyroxine report feeling tired, gaining weight, or having brain fog every time their generic changes. Their TSH levels swing out of range. It takes weeks to stabilize the dose again. One patient on Drugs.com wrote: "Every time my levothyroxine manufacturer changes, I feel terrible for weeks until my doctor adjusts my dose. It’s exhausting."
Warfarin is even trickier. It’s dosed by blood test - INR levels. A change in generic can cause your INR to jump or drop. That means risk of stroke or dangerous bleeding. The FDA recommends sticking with the same manufacturer for warfarin. But many pharmacies don’t track it.
For transplant patients on tacrolimus, switching generics can mean rejection. One study found that 15% of transplant patients had a drop in drug levels after a generic switch - enough to trigger organ damage.
What Patients Are Reporting
Surveys show mixed results. About 68% of patients say they notice no difference after switching generics. But for others, the impact is real.
- 44% of epilepsy patients report breakthrough seizures after switching generic antiepileptics.
- 33% of thyroid patients say their symptoms return after a manufacturer change.
- One Reddit user shared: "My seizure med switched from Mylan to Teva. Two breakthrough seizures in a month. My neurologist checked my blood - levels had dropped 30%."
Meanwhile, people on statins or lisinopril rarely report issues. Their bodies handle the variation. But if you’re on an NTI drug, you’re not just a statistic - you’re the 22% who feel the difference.
Why You Might Not Know It’s Happening
Most patients identify their meds by how they look. A blue oval pill. A red capsule. A white tablet with "5" on it. When the generic changes, the pill changes. But pharmacies don’t warn you. Your doctor might not even know.
A 2023 AMA survey found that 62% of doctors didn’t find out about generic switches until patients came in with problems. That’s because insurance companies make the switch - not the prescriber. And pharmacists aren’t required to notify anyone.
Worse, 11.5% of patients accidentally take two versions of the same drug because they didn’t recognize the new pill. They think the old one ran out. They refill it again. Now they’re taking double the dose.

What You Can Do
You don’t have to be powerless in this system. Here’s how to protect yourself:
- Ask your pharmacist - every time you refill - "Is this the same manufacturer as last time?" If it’s not, ask if you can stay on the same one.
- Request "dispense as written" on your prescription for NTI drugs. This tells the pharmacy not to substitute. Some insurers still override it, but it’s your first line of defense.
- Check your pill. Take a photo of your pill the first time you get it. Compare it next refill. If it looks different, ask why.
- Track your symptoms. If you’re on levothyroxine, warfarin, or an antiepileptic, keep a log. Note how you feel each week. If you start feeling off after a refill, it might be the switch.
- Ask your doctor about "lock-in" programs. Some hospitals and clinics have programs that lock your prescription to one generic manufacturer for the duration of your treatment. Ask if yours offers it.
What’s Being Done
Regulators are starting to pay attention. In June 2024, Medsafe (New Zealand’s drug regulator) issued new guidance saying levothyroxine should not be switched between brands unless absolutely necessary. The FDA launched a pilot program in 2023 requiring generic makers to report major formulation changes. And in 2024, the Association for Accessible Medicines announced a plan to standardize pill appearance across generic manufacturers to reduce confusion.
But progress is slow. For now, the system still prioritizes cost over consistency - especially for patients on high-risk drugs.
Bottom Line
Generic drugs save billions. That’s good. But assuming all generics are the same? That’s dangerous. For most people, switching doesn’t matter. For others - especially those on thyroid, blood thinner, or seizure meds - it can be life-changing.
If you’re on a narrow therapeutic index drug, don’t let a pharmacy decision become your health risk. Be informed. Be vigilant. Ask questions. Your body doesn’t care about the label on the bottle. It only cares about what’s inside - and whether it’s the same as last time.
Can I ask my pharmacy to always give me the same generic manufacturer?
Yes. You can ask your pharmacist to use the same manufacturer each time. Some pharmacies will accommodate this, especially if you’re on a narrow therapeutic index drug like levothyroxine or warfarin. You can also ask your doctor to write "dispense as written" or "do not substitute" on your prescription. This legally prevents substitution - though some insurance plans may still try to override it. If they do, you can appeal or pay out-of-pocket for the preferred version.
Why do generic pills look different every time?
Each generic manufacturer uses different inactive ingredients - like dyes, fillers, and coatings - to make their version. These affect the pill’s color, shape, and size. Because the FDA only requires the active ingredient to match, manufacturers are free to change the appearance. That’s why your pill might be white one month and blue the next. It’s still the same drug, but not the same pill.
Is it safe to switch between generics for blood pressure or cholesterol meds?
For most people, yes. Drugs like lisinopril, atorvastatin, and metoprolol have wide therapeutic windows. Small changes in blood levels don’t usually cause problems. Studies show fewer than 10% of patients on these drugs report issues after switching generics. But if you’ve ever felt different - dizzy, tired, or out of sorts - after a refill, it’s worth mentioning to your doctor. Everyone’s body reacts differently.
What should I do if I think a generic switch caused side effects?
First, check your pill. Compare it to the last one you took. If it looks different, that’s a clue. Next, contact your doctor or pharmacist. Don’t stop your medication - but ask if the manufacturer changed. For NTI drugs like warfarin or levothyroxine, your doctor may order a blood test (INR or TSH) to check your levels. If levels are off, they can adjust your dose or switch you back. Document when symptoms started - it helps prove the connection.
Are there any drugs that should never be switched between generics?
Yes. The FDA and experts recommend avoiding switches for drugs with a narrow therapeutic index. This includes levothyroxine, warfarin, tacrolimus, cyclosporine, phenytoin, and carbamazepine. Even small changes in blood levels can lead to treatment failure or toxicity. Some health systems have "lock-in" policies for these drugs, meaning you get the same manufacturer for the entire course of treatment. Ask your doctor or pharmacist if your medication falls into this category.

Jay Ara
December 26, 2025 AT 19:53Been on warfarin for 8 years. Switched generics last year and my INR went nuts. Took 3 weeks to stabilize. Pharmacist didn’t say a word. Just handed me a different pill. Don’t trust the system.
Michael Bond
December 26, 2025 AT 20:22My mom switched levothyroxine brands and started gaining weight like crazy. Doctor finally figured it out. Don’t let this slide.
Angela Spagnolo
December 28, 2025 AT 09:54I… I didn’t even know this was a thing. Like… really? People are just… getting different pills? And no one tells you? That’s… scary. I mean… like… wow.
Zina Constantin
December 28, 2025 AT 14:36As someone who’s lived with hypothyroidism for 15 years, I can tell you this isn’t theoretical. I keep a photo of my pill on my phone. Every refill. Every. Single. Time. One month it’s a tiny white oval with a line down the middle. Next month? Big blue capsule with a star. I feel like a different person. Brain fog. Fatigue. Weight gain. My TSH swings like a pendulum. I’ve had to beg my doctor to write ‘dispense as written’ - and even then, my insurance fought it. This isn’t about cost savings. It’s about patient safety. If you’re on levothyroxine, warfarin, or seizure meds - don’t wait until you’re hospitalized to speak up. Be the annoying patient. Ask. Document. Fight. Your life depends on consistency - not corporate bids.
Kuldipsinh Rathod
December 29, 2025 AT 08:52My cousin on tacrolimus after transplant got switched and almost lost the kidney. Took 6 months to get back to normal. Pharmacist didn’t even know it was dangerous. Just did what the computer said.
SHAKTI BHARDWAJ
December 30, 2025 AT 23:29Oh please like the FDA is gonna fix this? They’re paid off by big pharma. You think they care about your thyroid? They care about profits. Stop being naive. This is capitalism. You’re a number. Your pill is a commodity.
Matthew Ingersoll
December 31, 2025 AT 03:31My pharmacy doesn’t even ask if I want the generic. They just hand it over. I’ve had to start asking specifically for Mylan’s levothyroxine. Now they know me. I’m the weird guy who cares about pill color.
carissa projo
January 1, 2026 AT 20:02Imagine if your car’s engine was swapped every time you filled up - same fuel, same model, but different spark plugs, different pistons, different timing. Would you drive it? Would you trust it? That’s what we’re doing with NTI drugs. We treat human biology like a vending machine: ‘Any version will do.’ But our bodies aren’t interchangeable parts. We’re complex, delicate systems. And yet we outsource our health to algorithms that optimize for $2.50 instead of $5. We need to stop normalizing this. It’s not ‘just a pill.’ It’s your rhythm, your stability, your life. If you’re on a narrow therapeutic index drug, you’re not being paranoid - you’re being intelligent. And you deserve better than a pharmacy’s inventory spreadsheet.
josue robert figueroa salazar
January 3, 2026 AT 16:00Most people don’t notice. So why make a fuss? You’re overreacting.
david jackson
January 5, 2026 AT 05:45Let me tell you what happened to my sister. She was on phenytoin for 12 years. Same manufacturer. Same pill. Same life. Then one day - boom - generic switch. No warning. No note. Just a different-looking tablet. Two weeks later - grand mal seizure. In the ER. No history of seizures. No triggers. No alcohol. No sleep deprivation. Just a different pill. The blood test showed her phenytoin level had dropped 40%. The neurologist said, ‘This happens more than you think.’ She’s fine now - stabilized on the old brand - but she’s terrified. And I’m furious. Why isn’t this mandated? Why isn’t there a barcode on the bottle that tells you the manufacturer? Why isn’t there a federal registry for NTI drug consistency? We have tracking for coffee beans but not for life-saving meds? This isn’t just a gap in the system - it’s a moral failure.
Jody Kennedy
January 6, 2026 AT 15:00Just started taking levothyroxine. I’m already checking the pill every time. Taking photos. Writing down how I feel. I’m not waiting to feel awful to act. This is my body - I’m taking control.
Sarah Holmes
January 7, 2026 AT 05:50While I appreciate the anecdotal evidence presented, one must consider the broader pharmacoeconomic context. The FDA’s bioequivalence standards, while imperfect, are grounded in statistically significant clinical trials involving thousands of patients. To elevate individual variability - often attributable to nonadherence, comorbidities, or placebo effects - to the level of systemic crisis is not merely misleading, it is dangerously irresponsible. The cost savings generated by generic substitution have enabled millions of low-income patients to access essential therapeutics. To dismantle this system on the basis of emotional testimony is to prioritize the comfort of the few over the survival of the many. We must not confuse correlation with causation - nor allow sentiment to override evidence-based policy.