Pain Catastrophizing: CBT Tools to Reduce Distress

When your pain feels like it’s taking over your mind-when every twinge makes you think “This will never get better,” or “I can’t handle this anymore,”-you’re not just feeling physical discomfort. You’re caught in a cycle called pain catastrophizing. It’s not weakness. It’s not imagination. It’s a real, measurable pattern of thought that makes pain feel worse, last longer, and steal more from your life than the injury or condition alone ever could.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing isn’t just being upset about pain. It’s when your brain gets stuck in three specific thought loops: rumination (can’t stop thinking about the pain), magnification (assuming the worst-“This means I’m going to be disabled”), and helplessness (“There’s nothing I can do about it”). Research from the 1990s, led by Dr. Mick Sullivan, created the Pain Catastrophizing Scale (PCS) to measure this. It’s a simple 13-question tool. If your score is 30 or higher, you’re in the clinically significant range. That means your thoughts are actively making your pain worse-not just reflecting it. And it’s not just in your head. Brain scans show that when you catastrophize, areas linked to emotion and threat detection light up more intensely. Your body actually feels more pain because your mind is screaming danger. This isn’t “all in your head” as some dismissively say. It’s your brain’s alarm system stuck on maximum.Why CBT Works When Other Treatments Don’t
Medications, injections, even surgery can help with the physical side of pain-but they rarely touch the mental spiral. That’s where Cognitive Behavioral Therapy (CBT) steps in. It doesn’t pretend the pain isn’t real. It just helps you change how you respond to it. A 2023 review by the International Association for the Study of Pain found that CBT is the most effective treatment specifically for reducing catastrophizing. When studies focused only on people with high PCS scores, CBT outperformed all other therapies-including exercise alone. The best results? Combining CBT with movement. People who did both saw pain intensity drop by nearly half in just 12 weeks. One study followed a 45-year-old woman with fibromyalgia. Her PCS score was 42-severe catastrophizing. After 12 weeks of CBT, it dropped to 18. Her pain intensity fell by 50%. She went back to part-time work. She wasn’t cured. But she got her life back.The Three Core CBT Tools You Can Start Using Today
CBT isn’t magic. It’s a set of practical tools. You don’t need a therapist to begin using them-even if working with one gives better results.1. Self-Monitoring: Track Your Thoughts Like a Scientist
Start a simple journal. Every time pain spikes, write down:- What happened right before the pain got worse? (e.g., stood up too fast, forgot to stretch)
- What thought popped into your head? (e.g., “This is it. I’m ruined.”)
- How did you feel emotionally? (anxious? hopeless? scared?)
- What did you do? (avoided moving? screamed? canceled plans?)
- What was the actual physical sensation? (sharp? dull? throbbing?)
2. Cognitive Restructuring: Challenge the Worst-Case Script
Once you spot a catastrophic thought, ask yourself:- Is this thought based on facts-or fear?
- What’s a more realistic version of this?
- Have I felt this way before and survived?
Catastrophic thought: “If I walk the dog, I’ll be in bed for three days.”
Realistic rewrite: “Walking the dog might make my back ache for a few hours, but I’ve done it before. I’ll rest after, use my heat pack, and take it slow.”
This doesn’t mean lying to yourself. It means replacing the worst-case fantasy with a more accurate, manageable version. The goal isn’t to be positive. It’s to be accurate.3. Behavioral Activation: Move Even When You Don’t Want To
Avoidance feeds catastrophizing. The less you do, the more your brain believes you can’t do anything. CBT pushes back gently. Start tiny. If you used to walk 20 minutes but now avoid it, try 3 minutes. Set a timer. Walk around the block. Sit in the garden. Do one dish. Then rest. Celebrate the action-not the outcome. A 2024 study showed that patients who consistently did small activities-even when in pain-showed the fastest reduction in catastrophizing. Why? Because your brain learns: “I did it. I’m still here. I’m not broken.”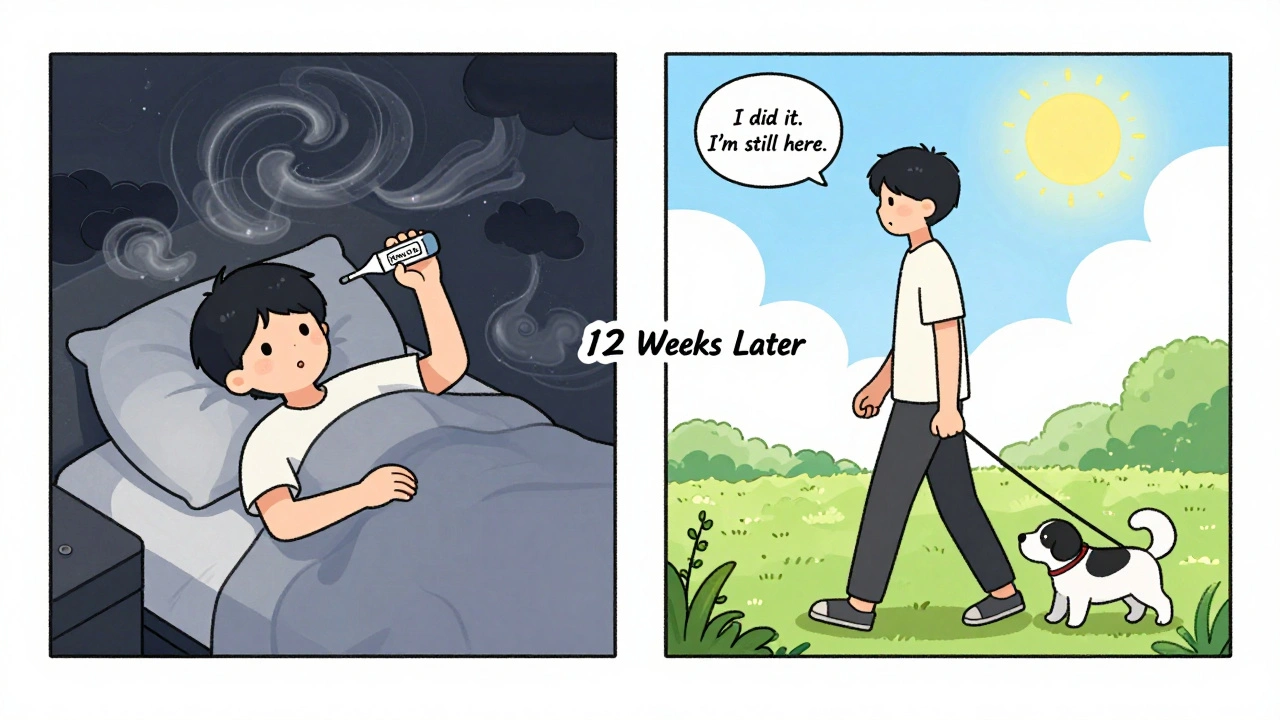
What Doesn’t Work-and Why People Quit
Many people try CBT and quit because they expect instant relief. It doesn’t work like painkillers. You won’t feel better after one session. It takes 3-4 weeks just to notice your catastrophic thoughts. Six to eight weeks to change them. One Reddit user, u/PainWarrior42, said: “I almost quit at week 4. I thought it wasn’t working. Then I looked back at my journal-I hadn’t canceled a single plan in two weeks. I didn’t realize I’d changed.” Dropout rates are around 22%. The main reason? “I didn’t see results fast enough.” Another challenge: when pain is at an 8 or 9 out of 10, your brain is too overloaded to think clearly. That’s normal. Don’t try to use CBT tools during a flare-up. Wait until it drops to a 5 or 6. Then practice. Build the skill for when you need it most.Who Benefits Most-and Who Might Need More
CBT works best for people who:- Have chronic pain (not acute injury)
- Feel stuck in fear and helplessness
- Are willing to write things down and reflect
- Have some mental energy left-even if it’s small

The Future: Apps, Dashboards, and Micro-Interventions
You don’t need weekly therapy anymore. Digital tools are making CBT more accessible than ever. The U.S. Veterans Health Administration rolled out a Pain Management Dashboard across all its centers in late 2024. It tracks PCS scores, activity levels, and thought patterns automatically. Early results? A 32% drop in catastrophizing among 4,500 veterans. Apps like Curable and PainScale now offer guided CBT exercises you can do in 10 minutes a day. One new feature? A “catastrophe alert” that sends a calming audio prompt when you log a high-pain episode-reminding you to pause, breathe, and reframe before the spiral begins. By 2025, 75% of pain clinics will screen for catastrophizing routinely. That means if you walk into a pain clinic, they’ll ask you the PCS questions-just like checking your blood pressure.Getting Started: Your First Week Plan
You don’t need to do everything at once. Here’s a simple 7-day plan:- Download a free journal app or use a notebook.
- Each day, write down one time you had a strong pain spike. Note the thought, feeling, and action.
- On day 3, pick one catastrophic thought and rewrite it realistically.
- On day 5, do one small activity you’ve been avoiding-even if it’s just sitting outside for 5 minutes.
- On day 7, reread your journal. Look for patterns. Ask yourself: “Did I survive yesterday’s pain? Yes? Then I’m still capable.”
Pain might always be part of your story. But it doesn’t have to write the ending.
Is pain catastrophizing the same as being depressed?
No. While they often happen together, they’re different. Depression is a low mood, lack of energy, and loss of interest in life. Pain catastrophizing is a specific pattern of thinking about pain-focusing on it, imagining the worst, and feeling helpless. Someone can catastrophize without being depressed, and vice versa. But the two feed each other. Treating catastrophizing often lifts mood, even if depression is still present.
Can I do CBT for pain catastrophizing on my own?
Yes. Many people start with free apps, online workbooks, or journaling. Tools like self-monitoring and cognitive restructuring can be done alone. But working with a trained therapist-especially one experienced in chronic pain-doubles your chances of success. If you’re struggling to stick with it, or your pain is severe, find a psychologist who specializes in pain management.
How long until I see results from CBT?
Most people notice changes in their thought patterns after 3-4 weeks. A measurable drop in pain distress usually shows up by week 6-8. It’s not a quick fix. But the changes last. Unlike medication, CBT teaches you skills you keep using for years.
What if I can’t think clearly when my pain is bad?
That’s normal. Don’t try to use CBT tools during a flare-up. Wait until the pain eases to a 5 or 6 out of 10. That’s when your brain has enough space to practice. Think of it like training for a race-you don’t run a marathon when you’re injured. You build strength when you’re stable. Then, when the flare comes, you’re better prepared.
Are there free tools or apps I can use?
Yes. The VA’s Whole Health Library offers free CBT worksheets for pain catastrophizing. Apps like Curable and PainScale have free versions with guided exercises. You can also find printable pain journals online from the American Chronic Pain Association. Start with journaling-it costs nothing and builds the foundation for everything else.

ian septian
December 8, 2025 AT 18:16Just start journaling one thought a day. That’s it. No fancy apps. No pressure. Do it for a week. You’ll be surprised.
Lola Bchoudi
December 9, 2025 AT 22:18CBT for pain catastrophizing isn’t just ‘think positive’-it’s neuroplasticity in action. The PCS isn’t a personality test, it’s a biomarker of maladaptive cognitive-emotional looping. When you engage in cognitive restructuring, you’re literally downregulating amygdala hyperactivity and strengthening prefrontal top-down inhibition. This isn’t woo-it’s fMRI-validated. And the behavioral activation component? It’s exposure therapy disguised as walking the dog. You’re retraining the threat response system. Do it consistently, and you rewire the pain matrix.
Morgan Tait
December 11, 2025 AT 13:37They never tell you the real reason CBT works-because Big Pharma doesn’t profit from it. You think they want you to fix your pain with journaling and 3-minute walks? Nah. They want you hooked on opioids, nerve blocks, and spinal stimulators. That’s why insurance won’t cover CBT unless you beg. And don’t get me started on the VA dashboard-sounds like a surveillance tool disguised as help. They’re tracking your thoughts now. Welcome to pain dystopia.
Darcie Streeter-Oxland
December 11, 2025 AT 22:22While the conceptual framework presented is not without merit, I must express my reservations regarding the uncritical endorsement of CBT as a panacea. The methodological limitations of the referenced 2023 review, particularly the absence of long-term follow-up data and the potential for publication bias, render the conclusions somewhat tenuous. Moreover, the suggestion that individuals may self-administer CBT without professional oversight borders on the irresponsible, given the cognitive distortions inherent in the condition under discussion.
Sarah Gray
December 13, 2025 AT 14:09Oh please. You think writing down thoughts is going to fix fibromyalgia? People who do this stuff are just deluding themselves. Real pain doesn’t care about your journal. And if you’re ‘only’ at a 5 out of 10, you’re not in pain-you’re just lazy. I’ve had real pain. The kind that makes you cry in the shower. CBT is for people who don’t want to admit they need real medicine.
Andrea Petrov
December 14, 2025 AT 04:39Why do you think the VA rolled out that dashboard? It’s not to help you-it’s to monitor who’s ‘non-compliant.’ They’re using your PCS scores to ration care. If your score drops too fast, they assume you’re faking. If it stays high, they push you into mandatory ‘wellness’ programs that cost you your disability benefits. I’ve seen it happen. This isn’t therapy. It’s behavioral control dressed up as science.
Steve Sullivan
December 16, 2025 AT 02:43Bro, I did this for 6 weeks. Started with 3-minute walks. Wrote down one thought a day. Didn’t feel like much. Then one day I realized I’d gone 10 days without cancelling plans. I didn’t even notice. 😅 It’s like… your brain is a muscle. You gotta lift small weights before you can bench. Also, I cried during the first journal entry. Not because I was weak. Because I was finally honest. 🤍
George Taylor
December 17, 2025 AT 02:26...and yet... despite the 'evidence'... the dropout rate remains at 22%... which... statistically... indicates... that... for nearly a quarter of individuals... this... intervention... is... ineffective... or... insufficient... and... yet... the article... glosses... over... this... with... a... cheery... 'just... try... again'... tone... which... is... not... just... misleading... it's... dangerous...
Nikhil Pattni
December 17, 2025 AT 13:13Listen, I come from India where pain is just part of life, you don't need fancy Western therapy to deal with it. My grandma had arthritis for 50 years and never wrote a single journal. She just breathed, prayed, and kept moving. CBT is a luxury for people who have too much time and too little faith. In our culture, we don't analyze pain-we endure it with dignity. Also, why are all the studies from the US? Did they forget the rest of the world exists? And apps? Ha! Most people here don't even have smartphones. This feels like cultural imperialism wrapped in a bow.
William Umstattd
December 18, 2025 AT 11:41Let me be perfectly clear: if you’re relying on journaling and 3-minute walks to manage chronic pain, you’re not healing-you’re surrendering. You’re letting your body rot while you ‘reframe’ your thoughts. Real strength is pushing through the pain, not whispering to yourself that ‘it’s okay.’ I’ve worked construction with a herniated disc. I didn’t need CBT-I needed grit. And if your pain is so bad you need a therapist to tell you to walk the dog, maybe you should’ve stayed in bed.
Simran Chettiar
December 20, 2025 AT 08:04One cannot help but reflect upon the existential implications of pain catastrophizing as a phenomenon deeply embedded within the ontological condition of the human subject. Is not pain itself, in its most primordial form, an assertion of finitude? And to attempt to ‘restructure’ such an experience through cognitive techniques is, in essence, a form of epistemological violence-a refusal to acknowledge the sacred terror of embodiment. CBT offers not liberation, but a sanitized illusion of control. One must sit with the ache. One must let it speak. Not rewrite it. Not log it. Not analyze it. Simply… be with it. As the Zen masters say: ‘The wound is the place where the light enters you.’
Anna Roh
December 20, 2025 AT 12:00I tried this. For two weeks. Then my pain got worse. My therapist said I wasn’t ‘engaging enough.’ I stopped. Now I’m on meds. And honestly? I feel better. Maybe CBT works for some. But for me? It felt like being told to ‘just think happy thoughts’ while my spine was crumbling. I’m not mad. Just done.
Richard Eite
December 20, 2025 AT 19:36USA only. CBT? We don’t need it. We got grit. Pain? Man up. Walk it off. Stop whining. This is America. We don’t journal. We lift. We work. We suffer silently. If you need an app to tell you to walk the dog, you’re not disabled-you’re soft.
Kathy Haverly
December 21, 2025 AT 20:18So let me get this straight-you’re telling people with real, debilitating pain to write down their thoughts like they’re in middle school? And you call that treatment? You’re not helping. You’re gaslighting. If your pain is at an 8, you don’t need a ‘realistic rewrite.’ You need morphine. Or a damn doctor who listens. This isn’t self-help. It’s victim-blaming with a thesaurus.