Opioids: Understanding the Risks of Tolerance, Dependence, and Overdose

How Opioids Work - and Why They’re So Dangerous
Opioids are powerful painkillers that bind to special receptors in your brain and spine, blocking pain signals and triggering a flood of dopamine - the chemical behind pleasure and reward. That’s why they work so well for severe pain after surgery or cancer treatment. But that same mechanism is what makes them so risky. The brain doesn’t distinguish between pain relief and euphoria. Over time, it starts to rely on the drug just to feel normal.
There are six main opioids used in medicine: morphine, oxycodone, hydromorphone, fentanyl, buprenorphine, and methadone. Fentanyl is the most dangerous - it’s 50 to 100 times stronger than morphine. A tiny amount, smaller than a grain of salt, can stop your breathing. In 2021, synthetic opioids like fentanyl were involved in over 70% of all opioid overdose deaths in the U.S.
Tolerance: The Slow Trap
Tolerance doesn’t happen overnight. It creeps up. At first, a 10mg oxycodone pill eases your pain. After a few weeks, you need 15mg. Then 20mg. Your body adapts. The opioid receptors on your nerve cells become less responsive. They’re either internalized, phosphorylated, or downregulated - scientific terms for the brain saying, ‘I’ve had enough.’
Here’s the cruel part: tolerance to pain relief and euphoria develops faster than tolerance to respiratory depression. That means you can keep increasing your dose to feel the same high or control your pain, but your body never fully adjusts to the risk of stopping breathing. This mismatch is why even long-term users overdose. They think they’re ‘used to it.’ They’re not.
Dependence: When Your Body Demands the Drug
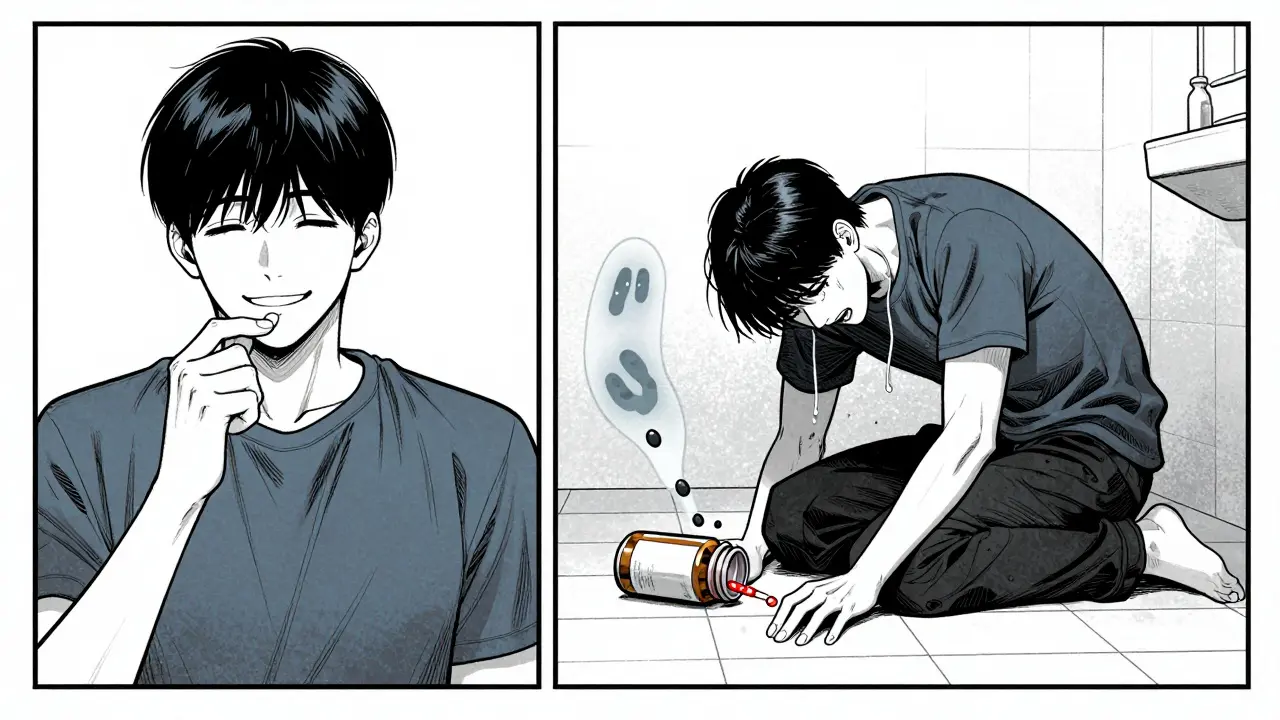
Tolerance leads to dependence. Your brain rewires itself to need opioids just to function. Without them, you don’t just feel bad - you get sick. Sweating, shaking, vomiting, diarrhea, bone pain, anxiety. It’s not weakness. It’s biology. Your nervous system has changed. You’re physically dependent.
Dependence doesn’t mean addiction, but it often leads to it. People don’t start using opioids to get high - they start for back pain, a broken bone, a dental procedure. Then they keep taking them because stopping feels worse than the original injury. By the time they realize they’re trapped, their body has already rewritten its rules.
Overdose: The Silent Killer
An overdose happens when opioids overwhelm your brain’s breathing center. Your lungs slow down, then stop. Oxygen drops. Brain damage begins in minutes. Death follows if no one intervenes.
Most people think overdoses only happen to people using heroin or street drugs. That’s outdated. Today, the biggest threat is fentanyl - often mixed into other drugs without the user’s knowledge. A pill bought as oxycodone might actually be fentanyl. One dose can kill.
But here’s what most don’t know: the biggest overdose risk isn’t new users - it’s people who’ve been clean. After weeks or months without opioids, your tolerance plummets. Your body forgets how to handle the drug. If you relapse and take your old dose - the one that used to work - you’re likely to die. Studies show 65% of opioid overdose deaths happen in people who had previously been in treatment. One Reddit user wrote: ‘After 6 months clean, I used my old dose and nearly died - paramedics said I was clinically dead for 4 minutes.’
Why Some Opioids Are Safer Than Others
Not all opioids are created equal. Buprenorphine is a partial agonist. It activates opioid receptors, but only up to a point. Even at high doses, it doesn’t cause the same level of respiratory depression as full agonists like fentanyl or oxycodone. That’s why it’s used in addiction treatment - it reduces cravings and withdrawal without the same overdose risk.
Methadone is a full agonist, but it’s long-acting. That makes it useful for maintenance therapy, but also dangerous if misused. Its effects can build up over days, especially when mixed with alcohol or benzodiazepines. Heroin’s danger comes from its unpredictable purity and the fact that it breaks down into three active metabolites - each processed differently based on your genes and what else you’ve taken.
Fentanyl? It’s not just strong - it’s unforgiving. A single miscalculation, a contaminated batch, a relapse after abstinence - any of these can be fatal. In 2021, fentanyl alone caused nearly 28,500 deaths in the U.S.

What Happens When You Stop - And Why It’s So Hard
Detoxing from opioids isn’t like quitting caffeine. It’s like your body is screaming for a drug it can’t live without. Withdrawal peaks around day 3 and lasts about a week, but the psychological craving? That can last months. That’s why most people relapse - not because they lack willpower, but because their brain still thinks it needs the drug to survive.
And here’s the irony: the longer you’ve used, the harder it is to quit - but the more dangerous relapse becomes. Your tolerance drops fast. Your risk of death spikes. That’s why harm reduction programs push for naloxone (Narcan) access for everyone who uses opioids - or knows someone who does. Naloxone reverses overdoses in minutes. It’s safe, easy to use, and saves lives.
What’s Changing - And What Still Needs to Change
In 2023, the U.S. passed the Mainstreaming Addiction Treatment (MAT) Act. This removed the old ‘X-waiver’ that only allowed 150,000 doctors to prescribe buprenorphine. Now, all 1.1 million licensed physicians can. That’s a game-changer. More people can get treatment without needing to find a specialist.
Prescription rates have dropped since their peak in 2012 - from 81 prescriptions per 100 people to 47. But the gap hasn’t been filled with safer alternatives. Instead, illicit fentanyl flooded the market. DEA seizures of fentanyl rose 1,200% between 2015 and 2022.
Pharmaceutical companies are now required by the FDA to educate patients on tolerance and overdose risk. New formulations like AVERSION technology make pills harder to crush or snort - but they don’t stop tolerance. The real hope lies in research on biased opioid ligands - drugs that relieve pain without triggering respiratory depression. That’s still years away.
For now, the best tools we have are: buprenorphine for treatment, naloxone for emergencies, and education for everyone. Because understanding tolerance isn’t just medical knowledge - it’s survival.
What You Need to Know Right Now
- If you’re prescribed opioids, ask your doctor about the lowest effective dose and shortest duration.
- Never mix opioids with alcohol, sleeping pills, or benzodiazepines - that combination kills.
- If you’ve been clean for weeks or months, never use your old dose again. Start with a fraction.
- Carry naloxone if you or someone you know uses opioids. It’s free in many pharmacies and community centers.
- Medication-assisted treatment (MAT) with buprenorphine or methadone cuts overdose risk by half.
The science is clear: tolerance isn’t a sign of strength. It’s a warning. Dependence isn’t moral failure. It’s neurobiology. Overdose isn’t always accidental - sometimes, it’s the inevitable result of a system that never taught people how dangerous this medicine really is.

Nicki Aries
February 2, 2026 AT 09:03People act like tolerance is some moral failing, but it’s just biology. Your brain adapts. That’s it. No judgment, just facts. And if you don’t get that, you’re part of the problem.
Bryan Coleman
February 3, 2026 AT 00:14just wanted to add that naloxone is way more accessible than people think. my local library gives it out for free, no ID needed. if you’re reading this and use opioids or know someone who does, go get some. it’s literally life or death. no exaggeration.