Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Opioid Adrenal Risk Calculator
How This Tool Works
Based on clinical evidence, this calculator estimates your risk of opioid-induced adrenal insufficiency using the key factors discussed in the article:
- Duration > 90 days
- Daily dose > 20 MME
- Long-acting opioids (methadone/fentanyl)
Your opioid therapy appears to be below key risk thresholds based on current evidence.
Recommendation: Continue monitoring symptoms like unexplained fatigue or low blood pressure.
Most people know opioids can cause constipation, drowsiness, or addiction. But few know they can quietly shut down your body’s stress response system - leading to a condition that can kill you if missed. Opioid-induced adrenal insufficiency isn’t a myth. It’s real. And it’s hiding in plain sight among patients on long-term pain meds.
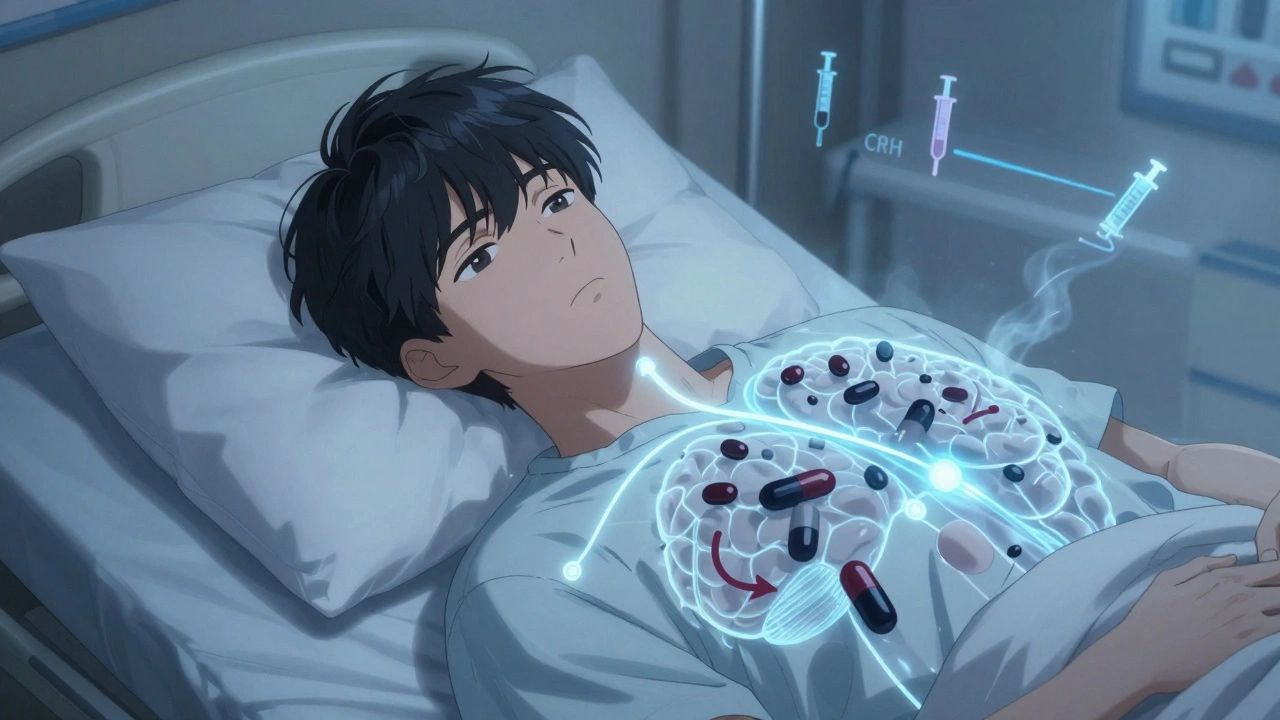
How Opioids Silence Your Stress Hormones
Your body has a built-in alarm system called the HPA axis - hypothalamus, pituitary, adrenal glands. When you’re stressed - whether from injury, infection, or surgery - this system kicks in. The hypothalamus sends a signal to the pituitary, which tells your adrenal glands to pump out cortisol. That’s your natural steroid. It keeps your blood pressure up, your blood sugar stable, and your immune system in check. Opioids don’t just block pain signals. They also bind to receptors in the brain that control this whole chain. Studies show they suppress the release of CRH (corticotropin-releasing hormone) and ACTH (adrenocorticotropic hormone). No ACTH? No cortisol. Even if your adrenal glands are perfectly healthy, they’re being told to sit still. This isn’t just theoretical. In a 2023 study of 162 adults on chronic opioid therapy, 5% had confirmed adrenal insufficiency. That’s one in every 20 people. And those numbers jump with higher doses. People taking more than 20 morphine milligram equivalents (MME) per day are at clear risk. Some studies found over 20% of long-term users failed adrenal stimulation tests - meaning their bodies couldn’t produce enough cortisol when pushed.Why This Gets Missed
The biggest problem? The symptoms look like everything else. Fatigue? Nausea? Low blood pressure? Weight loss? These are all common in people with chronic pain, depression, or cancer. Doctors assume it’s the disease - not the drug. A 25-year-old man in a 2015 case report was admitted for hypercalcemia after a critical illness. No one thought to check his cortisol levels until everything else failed. Turns out, his methadone had shut down his adrenal response. Once he stopped opioids and got replacement steroids, his calcium levels normalized. His body came back to life. Opioid-induced adrenal insufficiency doesn’t cause vomiting or dark skin like classic Addison’s disease. It’s subtler. It’s the quiet kind of failure. You don’t collapse in the ER. You just feel worse than you should. You don’t recover after surgery. You get sicker after a flu. You’re told it’s ‘just stress’ - when your body literally can’t respond to stress anymore.Who’s at Risk?
It’s not just heroin users or people on high-dose painkillers. It’s anyone on chronic opioid therapy - even if they’re following prescriptions. Risk factors are clear:- Taking opioids for more than 90 days
- Doses above 20 MME per day
- Using long-acting opioids like methadone or fentanyl patches
- Having other conditions that stress the body - like chronic pancreatitis, cancer, or recent surgery
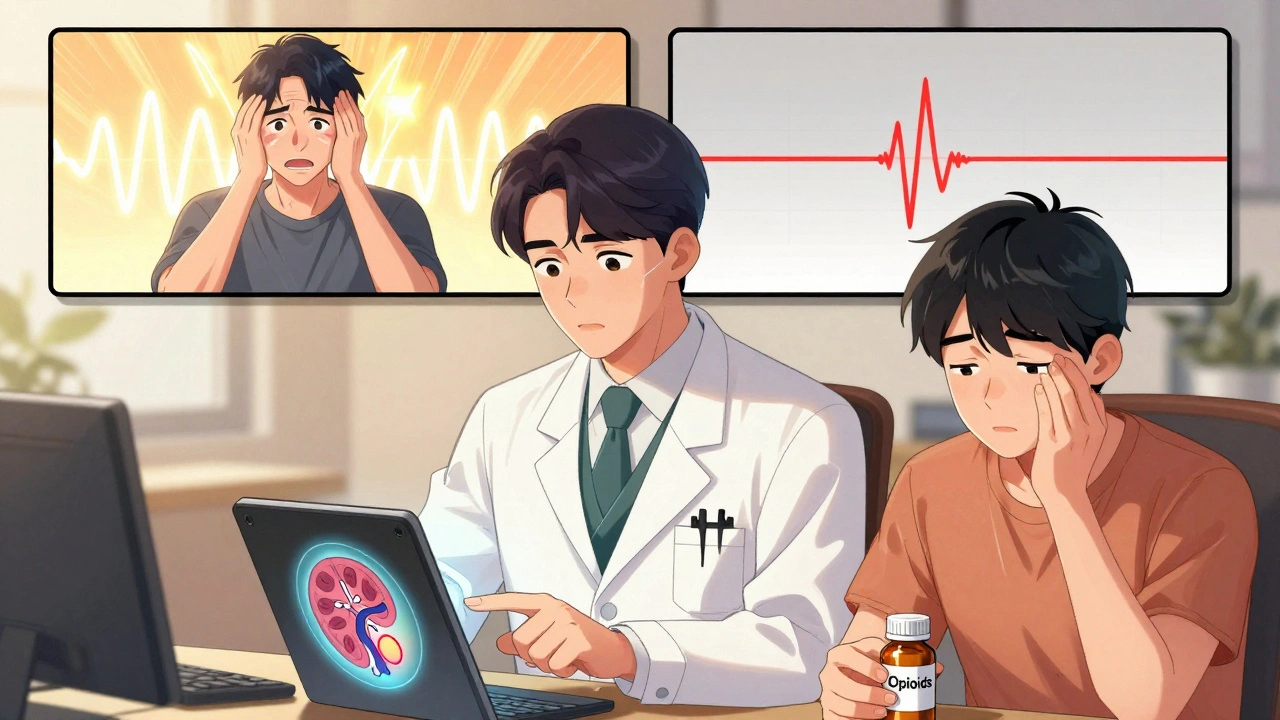
How It’s Diagnosed
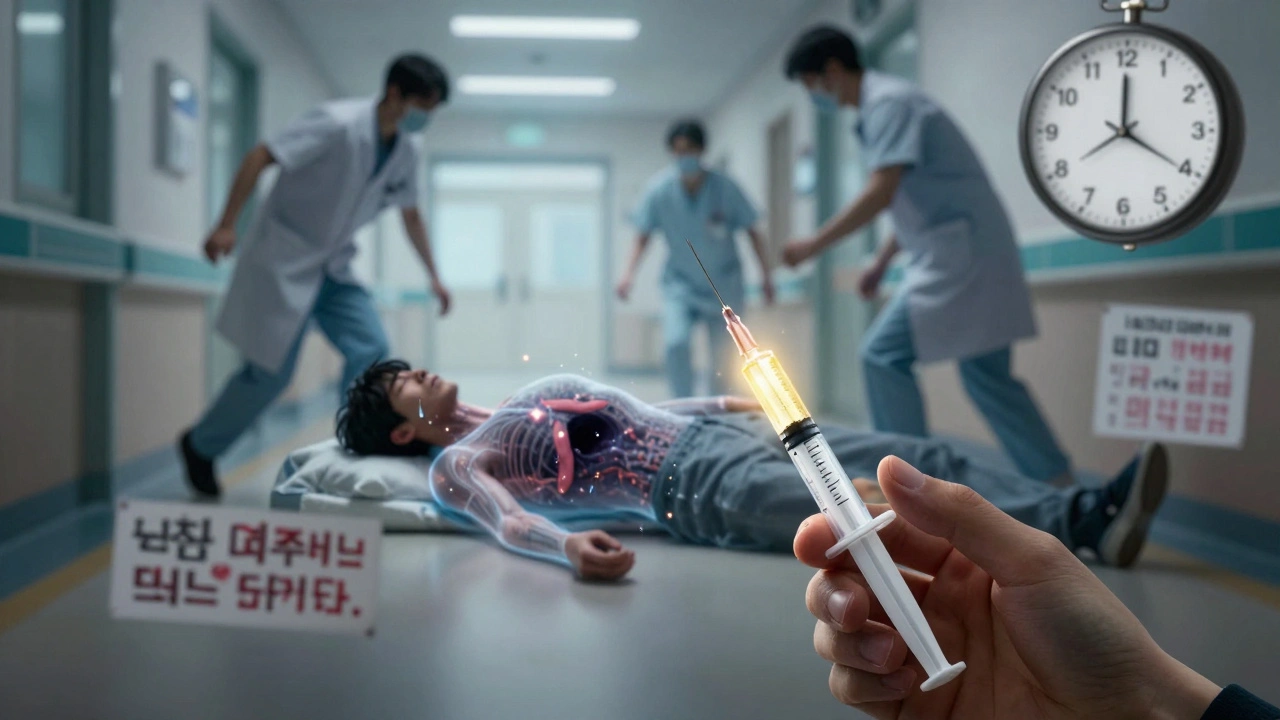
There’s no blood test you can order on a whim. But if you’re on long-term opioids and feel constantly drained, it’s worth asking. The gold standard is the ACTH stimulation test. You get a shot of synthetic ACTH. Then your cortisol is measured at 30 and 60 minutes. If your peak cortisol is under 18 mcg/dL (500 nmol/L), you likely have adrenal insufficiency. Some newer research suggests even lower thresholds - under 15 mcg/dL - may be more accurate for opioid users. A morning cortisol level under 3 mcg/dL is a red flag. But a normal morning level doesn’t rule it out. That’s why the stimulation test matters. It tests your reserve - not your baseline. Don’t rely on saliva or hair cortisol tests. They’re not reliable for this condition. Only serum cortisol after stimulation is validated.What Happens If It’s Left Untreated?
This isn’t a ‘maybe’ problem. It’s a ‘when’ problem. Imagine you’re on opioids for back pain. You get the flu. Your body needs cortisol to fight it. But your adrenal glands are turned off. You develop low blood pressure, vomiting, confusion. You’re rushed to the hospital. The doctors see infection. They give antibiotics. But you keep crashing. Without cortisol, your body can’t compensate. You go into adrenal crisis. Death can follow within hours. Studies show untreated adrenal insufficiency can lead to severe morbidity - and death. And it’s not rare in this population. With over 5% of the U.S. population on chronic opioid therapy, that’s millions of people at potential risk. Many of them will face a medical emergency at some point. If their adrenal insufficiency isn’t caught, they won’t survive it.Can It Be Fixed?
Yes. And that’s the good news. Opioid-induced adrenal insufficiency is reversible. In the 2015 case report, the 25-year-old man’s cortisol levels returned to normal after he stopped methadone. Other cases show similar results after tapering opioids. But here’s the catch: you can’t just stop cold turkey. If you’re already low on cortisol, suddenly removing opioids can trigger a crisis. That’s why treatment involves two steps:- Start glucocorticoid replacement (usually hydrocortisone) before or during opioid taper
- Slowly reduce the opioid dose under medical supervision
What Doctors Need to Do
This isn’t just a patient problem. It’s a system failure. Most pain clinics don’t screen for this. Most endocrinologists aren’t consulted until it’s too late. The AMA Ed Hub and other clinical guidelines now say: if you’re prescribing opioids long-term - especially above 20 MME - consider adrenal testing if the patient has unexplained fatigue, nausea, or low blood pressure. There’s no universal screening protocol yet. But the evidence is strong enough to act. If you’re on opioids for more than three months and feel constantly tired, ask your doctor for a morning cortisol test. If it’s low, push for the ACTH stimulation test. And if you’re a doctor: don’t assume fatigue is ‘just pain.’ Don’t assume low blood pressure is dehydration. Test. Rule it out. It’s simple. It’s cheap. And it can save a life.The Bigger Picture
We’re in the middle of an opioid crisis. Thousands die from overdose. But thousands more may be dying from complications we don’t even recognize. Opioid-induced adrenal insufficiency is a silent side effect. It doesn’t make headlines. It doesn’t show up in addiction statistics. But it’s real. And it’s preventable. The science is clear. The tools are available. What’s missing is awareness. If you’re on chronic opioids - whether for pain, cancer, or injury - know this: your body’s stress response might be turned off. And if you ever get sick, injured, or need surgery, that could be deadly. Ask for a cortisol test. Push for answers. Don’t wait for a crisis to find out you were at risk.What You Can Do Right Now
- If you’ve been on opioids for more than 90 days, track your symptoms: fatigue, dizziness, nausea, weight loss, low blood pressure
- Ask your doctor: ‘Could my opioids be affecting my adrenal glands?’
- Request a morning cortisol test - and if it’s low, ask for an ACTH stimulation test
- Never stop opioids suddenly - especially if you feel unwell
- If you’re scheduled for surgery, tell your anesthesiologist you’re on opioids

Mellissa Landrum
December 5, 2025 AT 16:22Mark Curry
December 7, 2025 AT 09:56😢
Manish Shankar
December 9, 2025 AT 02:31luke newton
December 9, 2025 AT 08:00an mo
December 9, 2025 AT 23:25aditya dixit
December 11, 2025 AT 05:42Mark Ziegenbein
December 12, 2025 AT 08:20we've replaced clinical observation with algorithmic prescribing and now we're surprised when the body rebels against the machine
opioids don't just silence your adrenal glands they silence your doctor's curiosity
and when your doctor stops asking why you're tired why you're nauseous why you're not recovering - that's when the real crisis begins
it's not about the dose it's about the disconnection
the system stopped seeing you as a person and started seeing you as a prescription number
and now you're paying with your survival
and no i'm not exaggerating this is the quiet apocalypse of modern medicine
we fixed pain but broke the body's ability to live
Juliet Morgan
December 12, 2025 AT 17:39