Occupational Lung Diseases: Silicosis, Asbestosis, and How to Prevent Them
Every year, thousands of workers breathe in dust and fibers they can’t see - and by the time they feel sick, it’s often too late. Silicosis and asbestosis aren’t rare accidents. They’re slow, silent killers that happen because safety measures were ignored, skipped, or never put in place. These diseases don’t show up overnight. They build up over years, sometimes decades, until the lungs are scarred beyond repair. And here’s the hard truth: silicosis and asbestosis are 100% preventable. Not 90%. Not “mostly.” 100%.
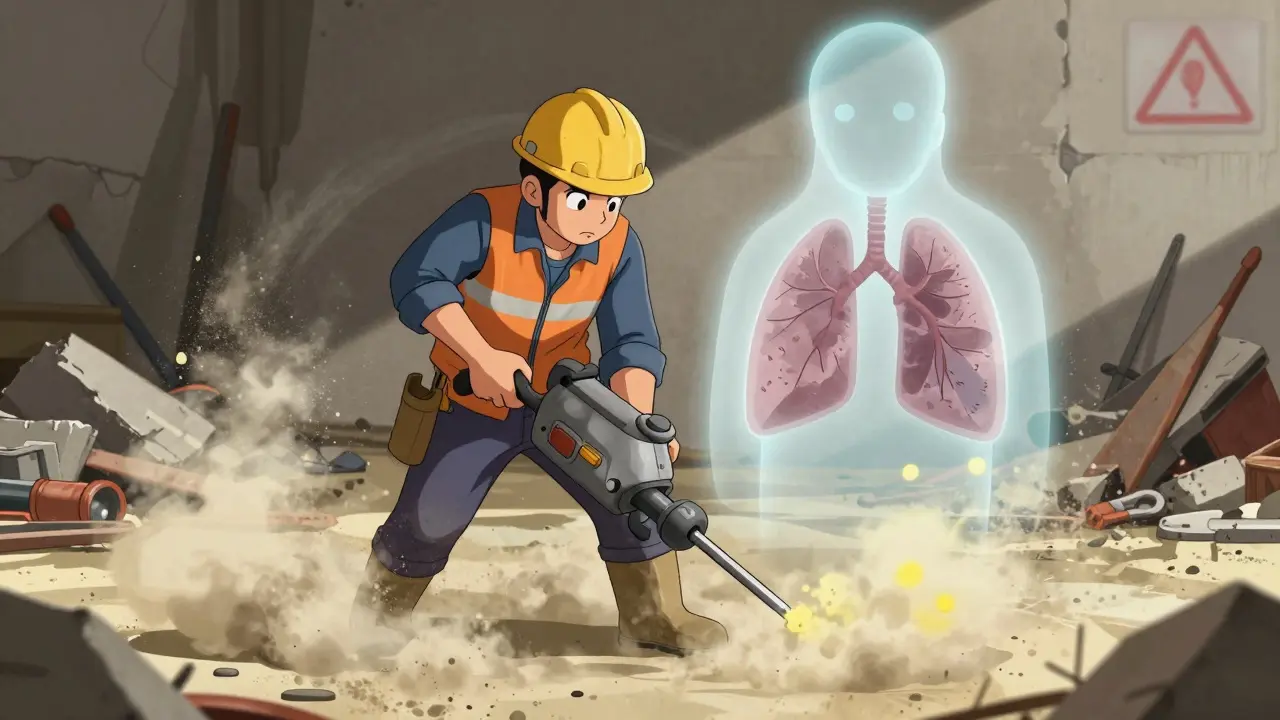
What Exactly Is Silicosis?
Silicosis happens when you breathe in tiny pieces of crystalline silica - a mineral found in sand, stone, concrete, and brick. Every time you cut, grind, drill, or sand these materials, you release dust that’s smaller than a red blood cell. Once it gets into your lungs, your body tries to fight it. But silica doesn’t break down. It stays. And over time, your lungs build scar tissue around it. That’s silicosis.
It’s not new. Ancient Egyptian stonecutters had it. So did 19th-century miners in Italy. Today, it’s still common in construction, mining, and manufacturing. In the U.S. alone, about 1,200 people die from silicosis each year. And the worst part? Workers are still being exposed because companies cut corners. Dry cutting of stone countertops? That’s a major source. Using a jackhammer on concrete without water? That’s a silent hazard.
Wet cutting - where water is sprayed right at the point of contact - reduces silica dust by up to 90%. Local exhaust ventilation on tools cuts exposure by 70-80%. But if you’re not using these methods, you’re gambling with your lungs.
What Is Asbestosis?
Asbestosis is caused by asbestos fibers - thin, needle-like particles once used in insulation, roofing, pipes, and floor tiles. When these materials are disturbed - during demolition, renovation, or even just aging - fibers float into the air. They get stuck in the lungs and cause scarring, just like silica. But asbestos is even more dangerous because there’s no safe level of exposure. Even a single fiber can, over time, trigger disease.
The first case was documented in 1906 in London, after an autopsy of a 33-year-old factory worker. Now, over a century later, asbestos is still in 733,000 public buildings in the U.S., according to the EPA. Many of them are schools, hospitals, and old factories. Workers doing repairs or removals are at high risk. And unlike silicosis, which can sometimes stabilize if exposure stops, asbestosis keeps getting worse even after you’re no longer exposed.
Asbestos is also linked to mesothelioma and lung cancer. The International Agency for Research on Cancer (IARC) classifies it as a known human carcinogen. No amount is safe. No exception.

Why Prevention Isn’t Just About Masks
Too many people think a simple N-95 mask is enough. It’s not. Respirators are the last line of defense - not the first.
The hierarchy of controls is clear:
- Elimination - Don’t use silica or asbestos at all. Replace with safer materials.
- Substitution - Use less hazardous alternatives (like quartz-free abrasives).
- Engineering Controls - Ventilation, wet methods, enclosed systems.
- Administrative Controls - Limit exposure time, rotate workers, training.
- PPE - Respirators, gloves, protective clothing.
Engineering controls reduce exposure by 80-90%. Administrative controls? About 50-70%. PPE? Only 40-60% - and only if it’s worn correctly, fit-tested, and maintained. Yet, in many workplaces, PPE is the only thing they offer.
OSHA requires annual fit testing for all respirator users. But a 2022 CDC report found that 68% of worker complaints about respirators were about discomfort - heat, pressure, fogging - and 32% of workers modified their masks to make them easier to wear. That means they’re not protected at all.
And here’s the kicker: smoking increases your risk of developing these diseases by 50-70%. If you’re exposed to silica or asbestos and you smoke, you’re not just at risk - you’re multiplying your risk.
What Real Prevention Looks Like
Prevention isn’t a poster on the wall. It’s a system.
In construction, wet cutting with water suppression is standard in many countries. In Australia, it’s required on all silica-generating tasks. In the U.S., OSHA’s 2016 Silica Standard made it mandatory for construction, but enforcement is spotty. In 2021, OSHA cited over 1,000 construction companies for silica violations - and fined them $3.2 million.
But money isn’t the issue. Culture is.
One Reddit user in r/Construction wrote: “My company got wet saws last year, but the foreman still yells at us for taking too long.” That’s the problem. If speed is valued over safety, workers will skip the water. They’ll skip the mask. They’ll take shortcuts - because they’re told to.
Successful prevention needs leadership. Supervisors must wear PPE 100% of the time. Workers need training that’s not just a 2-hour checkbox. The American Lung Association recommends 4-6 hours of initial training, with annual refreshers. Workers need to understand why it matters - not just what to do.
Small businesses struggle. In Wisconsin, 78% of companies with fewer than 20 employees had no formal respiratory protection program. They can’t afford $5,000 ventilation systems. But there are low-cost options: wet mopping instead of dry sweeping, using HEPA-filtered vacuums, sealing off work areas. These things cost less than one workers’ compensation claim.
Monitoring Is Your Early Warning System
By the time you’re coughing or out of breath, the damage is done. That’s why regular health checks are non-negotiable.
Spirometry - a simple breathing test - should be done at hire, then every five years for most workers. For those with existing lung conditions or high exposure, it should be done annually. Studies show early detection can slow disease progression by 30-50%.
The American Thoracic Society says this isn’t optional. It’s essential. And yet, most workplaces don’t do it. Why? Because it’s easier to ignore until someone gets sick.
Now, new tools are emerging. NIOSH’s Prevent eTool, launched in 2023, gives industry-specific guidance for 15 high-risk sectors. Early results show a 40% drop in respiratory incidents in companies using it. Wearable sensors that give real-time dust readings are also becoming more affordable. These aren’t sci-fi - they’re tools that can save lives.
The Bigger Picture
Occupational lung diseases account for 15-20% of all work-related illnesses in the U.S. Construction, mining, and manufacturing make up 75% of those cases. The global market for respiratory protection is growing - $7.8 billion in 2022, expected to hit $11.3 billion by 2027. That’s billions spent on masks, filters, and gear - while the root causes go unaddressed.
The European Respiratory Society says 60-70% of these diseases could be prevented with current technology. But technology alone won’t fix it. You need enforcement. You need training. You need accountability. You need a culture where workers can speak up without fear.
OSHA’s whistleblower protections exist for a reason. If you see unsafe conditions - a dry saw running, no ventilation, no fit test - you have the right to report it. And you should.
Because silicosis and asbestosis aren’t inevitable. They’re choices. Choices made by companies that prioritize profit over people. Choices made by managers who don’t know better. Choices made by workers who think they’re invincible.
But you don’t have to be part of that story. If you work with stone, concrete, insulation, or demolition - know the risks. Demand better. Use the water. Wear the mask. Get tested. Speak up.
Your lungs won’t thank you today. But they’ll thank you in 10 years - if you act now.

Randall Little
January 12, 2026 AT 23:03So let me get this straight - we’ve known since the 1800s that silica kills, yet we still let people sand drywall with a shop vac and call it ‘industry standard’? The only thing more terrifying than the disease is the corporate PowerPoint slide that says ‘Safety First’ right below the quarterly profit graph.
James Castner
January 14, 2026 AT 19:17The fundamental tragedy of occupational lung disease lies not in its biological mechanism - which, while insidious, is well-understood - but in the metaphysical collapse of moral responsibility within the industrial apparatus. When capital is prioritized over corporeal integrity, we do not merely neglect workers; we ontologically erase their humanity, reducing them to disposable variables in an algorithm of productivity. The N95 mask, often heralded as a panacea, is in fact a symbol of systemic failure - a Band-Aid on a hemorrhaging artery, a theological concession to the idol of efficiency. True prevention demands not merely engineering controls, but a radical reconfiguration of the social contract between labor and capital - one in which the dignity of breath is sacrosanct, not negotiable.
Adam Rivera
January 15, 2026 AT 11:37Man, I’ve seen this first hand. My uncle worked in demolition for 30 years, never wore a mask ‘cause it was ‘too hot.’ Last year he got on oxygen. Now he just sits on the porch, staring at the sky. If this post saves one guy from ending up like him, it’s worth it. Thanks for writing this.
Rosalee Vanness
January 16, 2026 AT 12:10I work in occupational health, and let me tell you - the most heartbreaking part isn’t the silicosis nodules or the fibrotic lungs. It’s the silence. The workers who come in for their annual spirometry test, smiling, saying ‘I’m fine,’ while their FEV1 is plummeting like a stone. They’ve been conditioned to believe that discomfort is part of the job. That ‘real men’ don’t complain. That ‘everyone does it.’ We need to flip that script. Not with posters. Not with mandatory training. But with stories. With voices. With accountability that doesn’t wait for a death certificate to act. Your lungs aren’t replaceable. And neither is your life. Please - if you’re reading this and you’re on a job site right now - stop. Breathe. Ask for the water spray. Demand the fit test. You’re not being slow - you’re being smart.
lucy cooke
January 17, 2026 AT 02:06Oh, how quaint. Another ‘educational’ treatise on the ‘silent killers’ of the proletariat - as if this were some new revelation unearthed by a 21st-century Socrates. The truth, darling, is that these diseases are merely the inevitable byproduct of a civilization that worships at the altar of progress while burying its conscience beneath concrete dust. The real tragedy? We’ve turned suffering into a content genre. ‘Silicosis: A Love Story’ - trending on TikTok next week. Meanwhile, the workers? Still breathing. Still dying. Still irrelevant.
John Tran
January 17, 2026 AT 22:49ok so like i read this whole thing and i think its so true but also kinda sad that people still dont get it like i work with my dad on a crew and he says ‘we been doin it this way since 87’ and i’m like dad the mask is not optional anymore but he just laughs and says ‘i got 30 years left’ but he coughs every morning and i just… i dont know what to say anymore. 😔
mike swinchoski
January 18, 2026 AT 02:11So you're telling me if you don't wear a mask you're a dumbass? Wow. Groundbreaking. My cousin died of lung cancer. He smoked. He worked construction. He didn't wear a mask. He made bad choices. Stop blaming companies. People choose to be lazy. Stop crying.
Angel Tiestos lopez
January 18, 2026 AT 22:07bro this hit different 😭 i work in tile install and we just got wet saws last month. the foreman still says ‘just go quick’ but now i spray the dust with a water bottle before i cut. not perfect, but better. also i told my buddy to get tested - he said ‘nah i’m fine’… i left him a N95 on his truck with a note: ‘you’re not invincible. -A’ 🤝
Robin Williams
January 20, 2026 AT 20:39Listen - I used to be the guy who thought ‘it won’t happen to me.’ Then I got a chest X-ray after a routine check-up. My lungs looked like a dried-up riverbed. I was 42. No symptoms. No cough. Just… scars. I quit construction. Started teaching. Now I talk to kids in trade schools. I show them my X-ray. I don’t beg. I don’t plead. I just say: ‘Your lungs don’t have an off switch.’ If you’re reading this and you’re still grinding dry - stop. Just stop. For five minutes. Breathe. Then ask for the water. You’re worth more than a paycheck.
Acacia Hendrix
January 22, 2026 AT 07:31The hierarchical model of control is conceptually sound but empirically inadequate in the context of neoliberal labor regimes. The very notion of ‘engineering controls’ presupposes a benevolent capital structure - one that is, by definition, antithetical to the profit-maximizing imperative. The PPE-centric paradigm is not an oversight; it is the logical endpoint of a system that externalizes bodily harm as a cost of production. The 40–60% efficacy of respirators is not a failure of implementation - it is a feature of the design. The solution lies not in better masks, but in the abolition of the wage-labor relation itself.
laura Drever
January 22, 2026 AT 17:28So what? People die. That’s life. You want safety? Don’t work in construction. Or mining. Or anywhere with dust. Stop whining. Also, your grammar is off. ‘Silicosis’ is spelled with an ‘i’ not an ‘e’. Just saying.
Damario Brown
January 23, 2026 AT 03:09you think this is bad wait till you see what happens when you breathe in asbestos AND smoke AND don't get checkups AND work 12 hour days AND have no insurance AND your boss says 'if you complain you're fired' AND you're undocumented AND your kid needs meds AND you're 58 AND your wife just left you AND your back is shot AND your lungs feel like sandpaper AND you still have to go to work tomorrow because there's no other option and you know what? you're not even mad anymore you're just tired. and that's the real disease.
Angel Molano
January 23, 2026 AT 20:10Wet cutting works. End of story. If you’re not using it, you’re a liability. And if your boss doesn’t enforce it, report them. OSHA doesn’t care about your ‘culture.’ They care about violations. And they’ll fine you into oblivion.
jefferson fernandes
January 24, 2026 AT 14:15Let’s be clear: this isn’t about ‘safety culture’ - it’s about power. Who gets to decide what’s ‘too expensive’? Who gets to say ‘we’ve always done it this way’? Workers aren’t the problem. The people who profit from their silence are. I’ve trained over 200 crews. I’ve seen foremen cry when they realize their brother died because they didn’t make them wear a mask. You don’t need a PhD to know this. You just need a heart. And the guts to say: ‘No more.’
Clay .Haeber
January 26, 2026 AT 07:26Oh, so now we’re all supposed to be lung health activists because some guy wrote a long post? Next you’ll tell me we should all meditate before operating a jackhammer. How about we just… let people make their own choices? If you want to wear a mask and spray water on every brick you cut - go ahead. But don’t lecture me because I don’t want to be a martyr for OSHA’s PR campaign. I’m not a statistic. I’m a worker. And I’ll breathe how I damn well please.