Medication Safety and Mental Health: How to Coordinate Care to Prevent Harm

When someone is managing a mental health condition like depression, bipolar disorder, or schizophrenia, their medication isn’t just another pill in the routine. It’s often the difference between stability and crisis. But here’s the hard truth: medication safety in mental health is one of the most overlooked areas in healthcare-and it’s putting lives at risk.
Think about this: a person on lithium for bipolar disorder needs regular blood tests to avoid kidney or thyroid damage. Yet, in England, only 40% of those prescribed lithium get those checks. In prisons, where mental illness is common, medication errors are 30% higher than in community clinics. Why? Because care gets broken into pieces. A patient leaves the hospital, goes to a GP, gets discharged into housing, maybe ends up in jail-and no one talks to anyone else about what meds they’re on, why, or what side effects to watch for.
Why Mental Health Medications Are Different
Not all drugs are created equal. A blood pressure pill might have one or two side effects. A psychotropic drug? It can change your mood, your energy, your appetite, your thoughts-and sometimes, it can make things worse before they get better. Medications like clozapine, lithium, and certain antipsychotics are called high-alert for a reason. They’re powerful. They need monitoring. And they’re easy to mess up.
Take lithium. It’s been used for decades to stabilize moods. But the window between a therapeutic dose and a toxic one is narrow. Too little? The person might spiral into mania or depression. Too much? They could end up in the ER with tremors, confusion, or kidney failure. That’s why NICE guidelines say serum levels should be checked every three months. Yet, in real life? Many patients never get tested. Why? Because their GP doesn’t know the protocol. Or they don’t have time. Or the system doesn’t remind them.
Then there’s polypharmacy. When someone is on five, six, even ten different meds-antidepressants, antipsychotics, sleep aids, painkillers, diabetes drugs-the risk of dangerous interactions skyrockets. One study found that nearly half of people with serious mental illness are on three or more psychotropic drugs. Combine that with over-the-counter supplements, herbal remedies, or street drugs, and you’ve got a recipe for disaster. A patient might take melatonin for sleep, but it can amplify sedation from an antipsychotic. Or they might use cannabis to self-medicate anxiety, which can trigger psychosis in someone on antipsychotics. No one asks. No one documents. No one connects the dots.
The Hidden Risks: Communication Breakdowns
Medication errors in mental health rarely happen because a nurse gave the wrong pill. They happen because no one knew the patient was switched from olanzapine to quetiapine six weeks ago. Or because the prison pharmacy didn’t get the discharge summary. Or because the GP didn’t know the patient was being treated for schizophrenia and thought the antipsychotic was for "behavioral issues."
Transitions are the deadliest moments. When someone moves from hospital to home, from jail to community care, from one clinician to another-their medication list gets lost. That’s where medicines reconciliation comes in. It’s not just a form. It’s a process. Every time a patient changes setting, someone must sit down and compare what they’re taking now with what they were taking before. What’s been added? What’s been stopped? Why? Is the dose right? Is it still needed?
New Zealand’s Health Quality & Safety Commission found that when this is done right, medication discrepancies drop by over 60%. But it only works if it’s mandatory. Not optional. Not "if we have time." And it must include the patient. Too often, they’re not asked: "What are you taking?" They’re just handed a script. But many won’t speak up. They’re scared. They don’t trust the system. Or they’ve been told their symptoms are "all in their head."
Technology Can Help-But Only If It’s Used Right
Electronic prescribing systems cut prescribing errors by up to 55%. That’s huge. No more illegible handwriting. No more confusion between similar-sounding drugs like sertraline and escitalopram. Alerts for drug interactions. Automatic dose limits for high-risk meds. These tools exist. But they’re not magic.
In Australia, the My Health Record system allows GPs, psychiatrists, and pharmacists to see what’s been prescribed. But only if everyone uses it. Many community mental health teams still rely on paper files. Some prisons still use handwritten scripts. And if the patient moves between states? The records don’t always follow. Even when the tech is there, it’s often underused because staff are overwhelmed. A nurse might have 20 patients to see in an hour. There’s no time to check every alert.
The real problem isn’t the system. It’s the workflow. Technology needs to be built into the rhythm of care-not bolted on as an afterthought.
Who’s Responsible? Everyone
Medication safety isn’t just the psychiatrist’s job. Or the pharmacist’s. Or the nurse’s. It’s everyone’s.
General practitioners often manage mental health meds for years, especially in rural areas. But many GPs have little training in psychiatric pharmacology. Dr. Sarah Ashcroft from King’s College London found that GPs frequently prescribe antidepressants off-label-for insomnia, agitation, or anxiety-without realizing the risks. Mirtazapine, for example, is sometimes used as a sleep aid. But it’s also highly sedating, addictive, and prone to diversion. People hoard it. Sell it. Use it to get high. And no one tracks it.
Pharmacists? They’re the last line of defense. A community pharmacist might spot that a patient is getting three different antipsychotics from three different prescribers. But if they don’t have access to the full picture, they can’t act. Clinical pharmacists embedded in mental health teams reduce errors by 25%. That’s proven. But most places still don’t have them.
And what about the patient? They need to be part of the team. Not just told what to take, but asked: "How’s this working for you?" "What side effects are you noticing?" "Are you taking it every day?" If they’re not heard, they’ll stop. Or hide it. Or take too much.
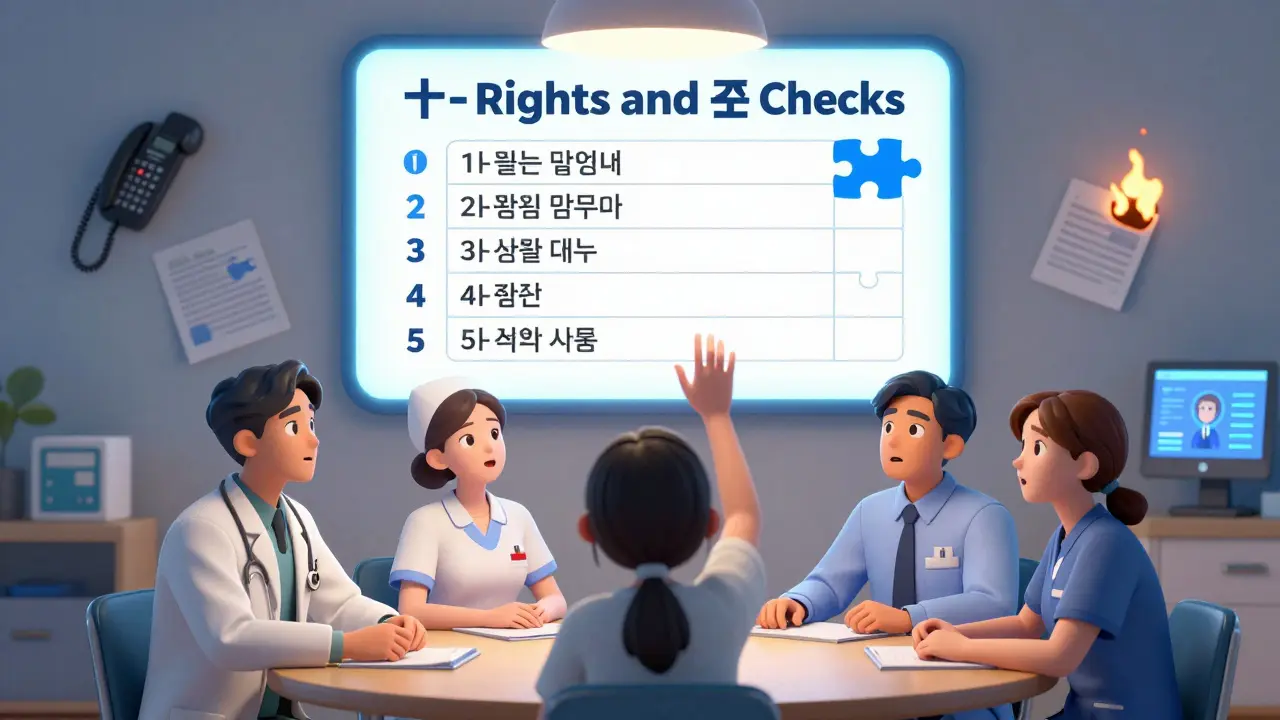
The Ten Rights and Three Checks: A Simple Framework
Saskatchewan’s Registered Psychiatric Nurses Association laid out a clear, practical system: the ten rights and three checks. It’s not fancy. But it works.
- Ten Rights: Right patient, right medication, right dose, right route, right time, right documentation, right reason, right response, right to refuse, right education.
- Three Checks: Check when you pull the med, check when you prepare it, check when you give it.
This isn’t bureaucracy. It’s a safety net. Every time a nurse hands over a pill, they pause. They verify. They ask. They document. And they make sure the patient understands why they’re taking it.
Imagine if every GP, every prison pharmacist, every community health worker used this. It wouldn’t fix everything. But it would stop a lot of avoidable harm.
What Needs to Change
There’s no single fix. But here’s what works, based on real evidence:
- Make medicines reconciliation mandatory at every transition. Hospital to home. Jail to clinic. Outpatient to crisis team. No exceptions.
- Embed clinical pharmacists in mental health teams. They’re not luxury add-ons. They’re safety officers.
- Train GPs on psychiatric meds. Not just how to prescribe, but how to monitor. What to watch for. When to refer.
- Use tech that talks. EHRs that sync across hospitals, GPs, pharmacies, and prisons. No silos.
- Track high-risk meds like lithium and clozapine. Set automatic reminders. Don’t rely on memory.
- Ask patients. Really ask. Not "Are you taking your meds?" But "How are you feeling on this?" "What’s hard about it?"
The Australian Medication Safety Standard says clinicians must "safely prescribe, dispense and administer appropriate medicines, and monitor medicine use." That’s the goal. But right now, too many systems are just checking boxes. Not saving lives.
What You Can Do
If you’re a patient or a family member:
- Keep a written list of every medication you take-name, dose, reason, who prescribed it.
- Bring it to every appointment. Even if you think it’s "just a check-up."
- Ask: "Why am I on this?" "What happens if I stop?" "Are there safer options?"
- Speak up if you’re not getting monitored. If you’re on lithium and haven’t had a blood test in six months, say something.
If you’re a clinician:
- Don’t assume someone else is managing the meds. Confirm.
- Use the ten rights and three checks. Every time.
- Document everything. Even the small stuff.
- Ask for help. If you’re unsure about a psychiatric med, call a psychiatrist or pharmacist. No shame.
Medication safety in mental health isn’t about perfection. It’s about consistency. It’s about remembering that behind every pill is a person trying to survive. And they deserve better than broken systems.
Why are psychotropic medications more dangerous than other drugs?
Psychotropic medications affect brain chemistry directly, which means small changes in dosage or timing can cause big shifts in mood, behavior, or cognition. Drugs like lithium and clozapine have narrow therapeutic windows-meaning the difference between an effective dose and a toxic one is very small. They also interact with other medications, alcohol, and even foods in ways that aren’t always obvious. Plus, patients with mental illness may have impaired judgment, memory issues, or communication barriers, making it harder to report side effects or follow instructions. This combination increases the risk of overdose, withdrawal reactions, or dangerous drug interactions.
What is medicines reconciliation and why does it matter?
Medicines reconciliation is the process of comparing a patient’s current medication list with what was prescribed before a transition-like leaving the hospital or moving from prison to the community. It’s designed to catch errors like missing drugs, wrong doses, or unnecessary repeats. Studies show it reduces medication discrepancies by up to 60%. Without it, patients often get discharged with incomplete or conflicting prescriptions, leading to hospital readmissions or even death. It’s not just paperwork-it’s a lifesaver.
Can electronic prescribing systems really reduce errors?
Yes. Evidence from New Zealand and other countries shows electronic prescribing cuts prescribing errors by 55%. It prevents illegible handwriting, reduces wrong-dose errors, flags dangerous interactions, and ensures dose limits are followed. But the system only works if everyone uses it consistently. If a GP uses e-prescribing but the prison pharmacy still uses paper, the safety net breaks. Technology helps-but only when integrated into real workflows.
Why is polypharmacy a problem in mental health?
Polypharmacy-using five or more medications at once-is common in mental health because patients often have coexisting conditions like diabetes, heart disease, or chronic pain. But mixing antidepressants, antipsychotics, sedatives, and painkillers increases the risk of side effects like dizziness, confusion, falls, and organ damage. Some combinations can even be fatal. For example, combining certain antipsychotics with opioids raises the risk of respiratory depression. The bigger issue? Many providers don’t review the full list. They treat one condition at a time, not the whole person.
What should I do if I think my mental health meds aren’t being managed safely?
Start by keeping a written list of every medication you take-including over-the-counter drugs and supplements. Bring it to every appointment. Ask your prescriber: "Is this still necessary?" "What are the risks if I stop?" "Have you checked my blood levels if I’m on lithium or clozapine?" If you’re not getting monitored, ask for a referral to a pharmacist or specialist. If you’re in a secure setting like a prison or hospital, request a medicines reconciliation. You have the right to know why you’re taking each drug and to be monitored for safety.

Sam Dickison
February 7, 2026 AT 16:49Let’s be real-lithium monitoring is a joke in primary care. I’ve seen patients on it for years with zero labs. GP’s got 12 back-to-back appointments and a 30-second window to review med lists. No one’s checking TSH or creatinine because no one’s got time, and the EHR doesn’t nudge them. It’s not negligence, it’s systemic collapse. We need automated alerts tied to billing cycles. If the lab doesn’t get done, the prescription auto-flags. No more "I forgot."