Managing SSRI Sexual Dysfunction: Dose Changes, Switches, and Adjuncts
SSRI Sexual Dysfunction Management Calculator
Your Current Situation
When you start an SSRI for depression, you expect to feel better. But for 35-70% of people, a new problem shows up: sexual dysfunction. It’s not rare. It’s not minor. It’s one of the most common reasons people stop taking their antidepressant. Reduced libido. Trouble reaching orgasm. Erectile issues. Dryness. These aren’t just inconvenient-they can wreck relationships, self-esteem, and your motivation to keep treating your depression.
Why This Happens
SSRIs work by boosting serotonin in the brain. That helps lift mood. But serotonin also shuts down sexual response pathways. The result? Your brain gets the signal to feel calm and safe-but not turned on. This isn’t a bug. It’s a direct effect of the drug’s mechanism. Symptoms usually start within the first 2-4 weeks. And here’s the twist: up to half of people with depression already have sexual problems before they even start the medication. So is it the illness? Or the pill? Often, it’s both.Option 1: Lower the Dose
Before you switch drugs or add something new, try cutting the dose. For many, especially those with mild or moderate depression, reducing the SSRI by 25-50% can improve sexual function without losing mood control. A 2023 study found this worked for 40-60% of patients. It’s simple: if you’re on 40mg of sertraline, try 20mg. If you’re on 20mg of escitalopram, try 10mg. Give it 2-3 weeks. Track your symptoms. If mood stays stable and sex improves? You’ve found your sweet spot.Option 2: Drug Holidays
This isn’t for everyone. But if you’re on an SSRI with a short half-life-like sertraline, citalopram, or escitalopram-you might benefit from a 48-72 hour break before planned sexual activity. Think of it like pausing the drug so your body can reset its sexual response. Studies show this helps 60-70% of people with delayed orgasm. But here’s the catch: fluoxetine (Prozac) has a half-life of over 14 days. A drug holiday won’t work. And if you stop abruptly, you risk withdrawal symptoms-dizziness, nausea, anxiety. About 15-20% of people get these. So only try this if you’re on a short-acting SSRI, and never skip doses randomly. Talk to your doctor first.Option 3: Switch Antidepressants
Not all SSRIs are created equal when it comes to sex. Paroxetine is the worst offender. Fluoxetine is next. Sertraline and escitalopram are better. But the real game-changer? Switching to a non-SSRI. Bupropion (Wellbutrin) is the most studied. It works on dopamine and norepinephrine, not serotonin. In trials, 60-70% of people saw major improvements in libido and orgasm. The catch? It takes 2-4 weeks to kick in. And if you have severe depression, switching away from an SSRI raises your relapse risk to 25-30%. Mirtazapine and nefazodone are alternatives. They block certain serotonin receptors and help with sex-but they make you sleepy. About 30-40% of users can’t handle the drowsiness.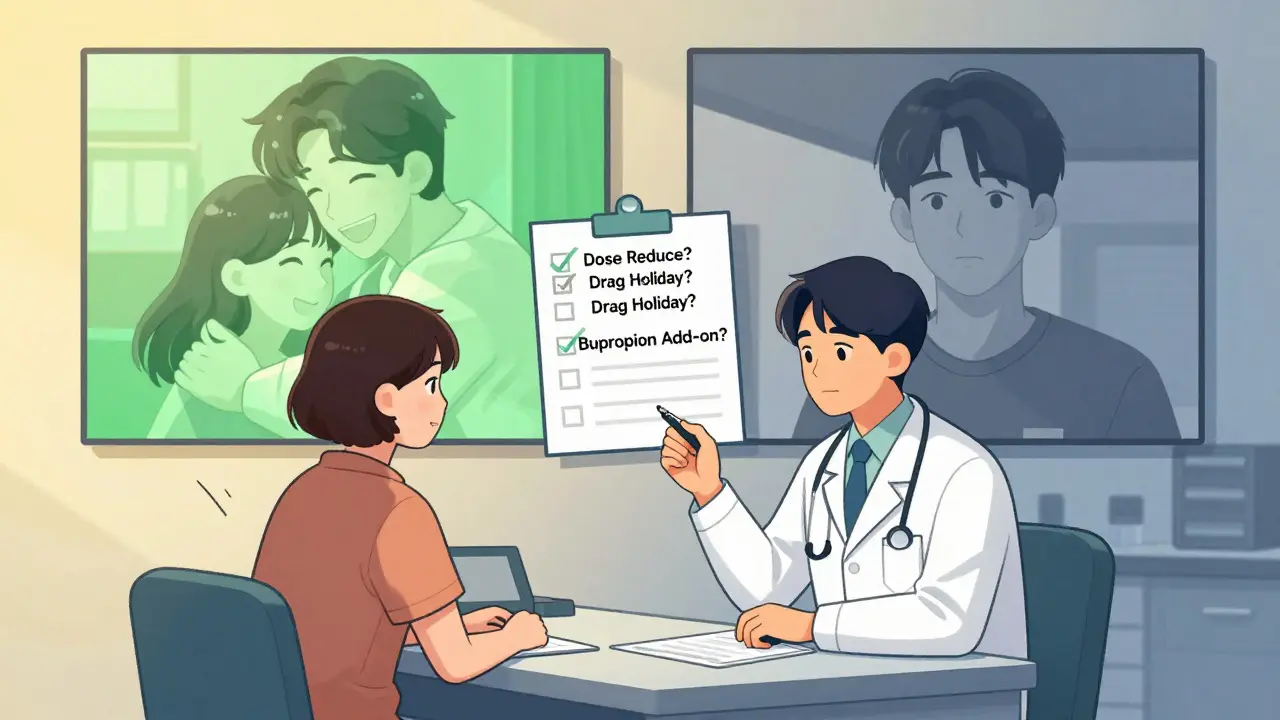
Option 4: Add Bupropion (The Best Evidence)
This is where the data gets strong. Adding bupropion to your SSRI doesn’t just help-it often fixes the problem. In a double-blind trial of 55 people on SSRIs like fluoxetine or paroxetine, daily bupropion (150mg twice a day) improved sexual desire and frequency in 66% of patients. That’s better than switching. As-needed bupropion (75mg taken 1-2 hours before sex) helped 38%. Not bad, but not as reliable. The downside? 20-25% of people get more anxiety, especially if they’re on fluoxetine. Start low: 75mg once daily for 3 days, then 75mg twice daily. Wait 4 weeks. If mood stays stable and sex improves? Keep it. If anxiety spikes? Talk to your doctor. This isn’t a magic pill-but it’s the most evidence-backed option we have.Other Adjuncts: What Works and What Doesn’t
There are other options, but they’re less reliable. Ropinirole and amantadine-dopamine boosters-can help in 40-50% of cases. But they can cause tremors or worsen anxiety. Buspirone (5-15mg daily) is a 5-HT1A partial agonist. It helps 45-55% of people with minimal side effects. But it takes 2-3 weeks. Cyproheptadine (2-4mg as needed) blocks serotonin and works in about half of users-but it’s sedating. And it’s not FDA-approved for this use. These are backup plans, not first-line.Behavioral Strategies Matter Too
Medication isn’t the whole story. Some of the most powerful fixes are non-pharmacological. Couples who tried “sensate focus” exercises-touching without pressure to perform-saw 50% improvement in satisfaction, even while staying on SSRIs. One therapist on Reddit said it best: “The problem isn’t always lack of arousal. It’s the dampening of pleasure.” Try new settings. New times of day. New ways of touching. Use lube. Watch erotic content. Increase stimulation. The goal isn’t to “cure” the SSRI effect. It’s to work around it.
What About Long-Term Side Effects?
In June 2023, Australia’s Therapeutic Goods Administration (TGA) warned about persistent sexual dysfunction after stopping SSRIs. Some people report symptoms lasting months-or years. A 2022 survey of SSRI users found 37% had ongoing issues after quitting. But here’s the debate: is this truly caused by the drug? Or are these people still depressed? A 2023 review of 19 studies concluded we don’t have enough solid data to say for sure. Only 2 studies were properly designed. The rest were observational. So yes, it’s possible. But we still don’t know how common it really is.What You Should Do Next
Don’t suffer in silence. If sex is suffering, talk to your doctor. Ask: “Is this a side effect of my medication?” Most doctors don’t bring it up. A 2023 poll found 73% of patients said their provider never mentioned sexual side effects before prescribing. That’s unacceptable. Start by tracking your symptoms. Use the Arizona Sexual Experience Scale (ASES)-it’s simple and validated. Rate your desire, arousal, orgasm, satisfaction. Do it monthly. If your score drops below 18, it’s time to act. First, try dose reduction. If that doesn’t work, consider bupropion augmentation. If you’re on fluoxetine, skip the drug holiday. If you’re on paroxetine, think about switching. And if nothing works, find a specialist. The Sexual Health Network lists over 1,200 clinicians trained in this exact issue.What’s Coming Next
New antidepressants are being developed to avoid this problem. Vilazodone and vortioxetine already have 25-30% lower rates of sexual side effects. But they cost $450/month-far more than generic sertraline at $10. And they’re not perfect. Meanwhile, a new drug called MK-0941, a 5-HT2C antagonist, showed 70% improvement in sexual function in a small 2023 trial-without hurting mood. It’s still in phase II, but it’s promising. The FDA is reviewing whether all SSRIs need stronger warnings. That’s coming. But for now, we have what we have: options. And you don’t have to choose between feeling better mentally and feeling better sexually.Can I just stop my SSRI to fix my sex life?
Stopping your SSRI abruptly can cause withdrawal symptoms like dizziness, nausea, brain zaps, and worsened depression. It also doesn’t guarantee your sexual side effects will go away-some persist even after stopping. Always taper under medical supervision. If you’re thinking about stopping, talk to your doctor about safer alternatives first.
Does bupropion help everyone with SSRI-induced sexual dysfunction?
No. About 20-25% of people experience increased anxiety or agitation when adding bupropion to an SSRI, especially fluoxetine. It works best for those with low libido or delayed orgasm, less so for erectile issues. Response varies by individual biology, dosage, and which SSRI you’re on. Track your symptoms for 4 weeks before deciding it’s not working.
Why do some SSRIs cause more sexual problems than others?
It comes down to how tightly the drug binds to the serotonin transporter and how long it stays in your system. Paroxetine binds very tightly and lingers longer, making it the worst offender. Fluoxetine has a very long half-life, so it builds up. Sertraline and escitalopram bind less tightly and clear faster, so they’re milder. Bupropion doesn’t affect serotonin at all, which is why it’s so helpful as an add-on.
Is there a test to know if my sexual dysfunction is from the SSRI or my depression?
There’s no blood test. But you can track it. If your sexual issues started within 2-4 weeks of beginning the SSRI, and you didn’t have them before, it’s likely medication-related. If you had low libido or orgasm problems before starting the SSRI, it’s probably depression. The Arizona Sexual Experience Scale (ASES) helps quantify changes over time. A drop of 5+ points on the scale after starting the SSRI strongly suggests drug-induced dysfunction.
How long should I wait before deciding a management strategy isn’t working?
Give each strategy at least 3-4 weeks. Dose changes take 2-3 weeks. Bupropion augmentation takes 2-4 weeks to reach full effect. Buspirone takes 2-3 weeks. Drug holidays require consistent timing over multiple cycles. Don’t quit too soon. But if you’re having severe anxiety, panic attacks, or worsening depression, stop and talk to your doctor immediately. Progress isn’t linear-but patience matters.
