IBD Surgery: Understanding Resection, Ostomy, and Postoperative Care

When Medical Treatment Isn’t Enough
For many people with Crohn’s disease or ulcerative colitis, medications eventually stop working. Symptoms like constant diarrhea, abdominal pain, bleeding, and fatigue don’t go away-even with biologics or immunosuppressants. When that happens, surgery isn’t a last resort; it’s often the best path to real relief. About 75% of Crohn’s patients and 15-30% of ulcerative colitis patients will need surgery at some point. The goal isn’t just to remove diseased tissue-it’s to restore your life.
What Does IBD Surgery Actually Involve?
IBD surgery isn’t one thing. It’s a set of procedures chosen based on your disease, where it’s located, and your overall health. The two main types are resection and ostomy.
Resection means cutting out the damaged part of your intestine and reconnecting the healthy ends. For Crohn’s disease, this often means removing a section of the small intestine (ileum) or colon. Surgeons try to preserve as much bowel as possible. A 2023 study from Cleveland Clinic showed that right colectomy for Crohn’s gives 60-70% remission at five years-but recurrence is common without ongoing treatment.
For ulcerative colitis, the standard is a proctocolectomy: removing the entire colon and rectum. This is the only cure for UC because the disease affects the whole colon. After removal, you have two options: a permanent ileostomy or an ileal pouch-anal anastomosis (IPAA), also called a J-pouch.
The J-Pouch: A Second Chance at Normal Bowel Function
The J-pouch is one of the most advanced procedures in modern IBD surgery. Surgeons take the last 8-10 centimeters of your small intestine, fold it into a J-shape, and attach it directly to your anus. This creates a new internal reservoir so you can pass stool naturally again.
It’s not a one-and-done procedure. Most J-pouch surgeries happen in three stages over several months. First, the colon and rectum are removed, and a temporary ileostomy is created. After 8-12 weeks, the pouch is built and connected to the anus. Then, after another 6-8 weeks of healing, the ileostomy is reversed. About 60% of patients need this temporary stoma to protect the new connection.
Success rates are high: 80-90% of people report satisfaction after J-pouch surgery, according to NYU Langone Health. Most have 4-8 bowel movements a day after recovery. But it’s not perfect. Up to 40% develop pouchitis-an inflammation of the pouch that often requires antibiotics. Some need additional surgeries to fix leaks, strictures, or fistulas.
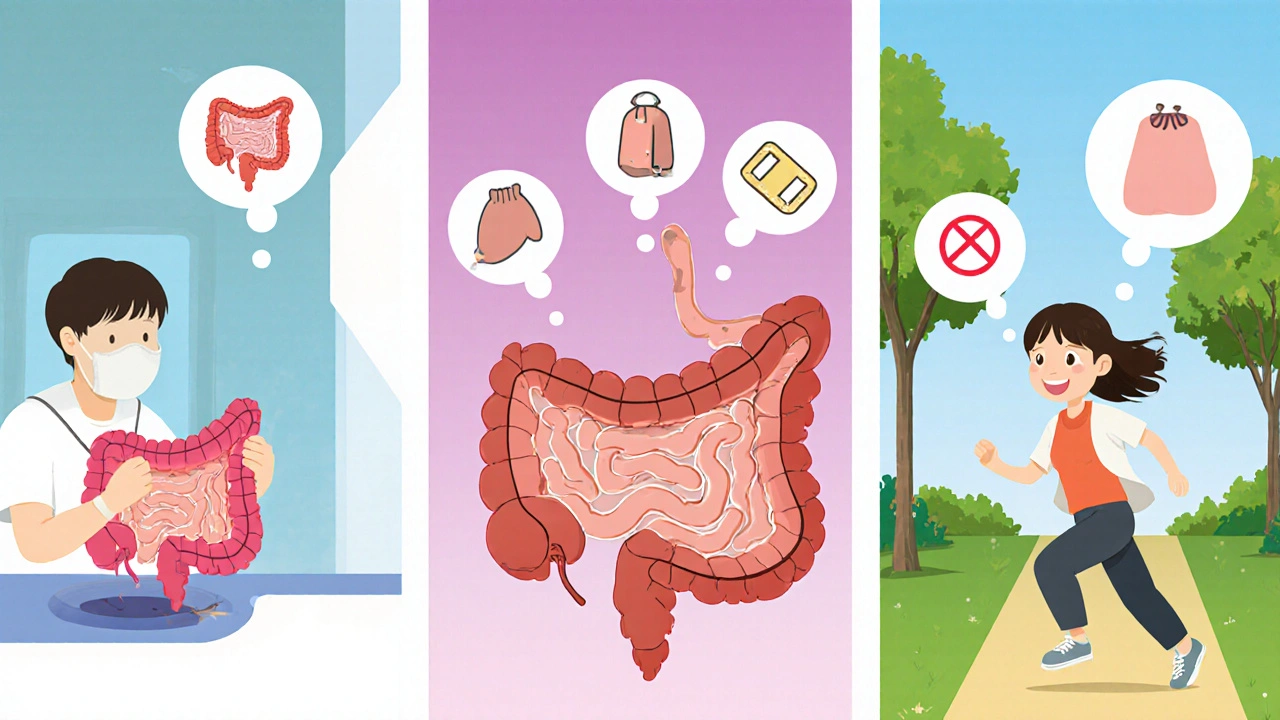
Ostomy: Living with an External Bag
An ostomy means creating an opening in your abdomen for waste to exit your body into a bag. This can be temporary or permanent. In IBD, it’s often an ileostomy-meaning waste comes from the small intestine.
The stoma is about the size of a quarter, sticking out 1-2 centimeters from your skin. You’ll need to empty the bag 4-6 times a day. It sounds daunting, but many patients say it’s life-changing. On Reddit’s r/IBD community, 65% of those with ostomies say they got immediate symptom relief. No more urgent bathroom runs. No more blood in stool. No more fear of public places.
But there are challenges. Skin irritation happens in 41% of negative reports. Body image issues affect 29%. That’s why training is critical. Certified wound, ostomy, and continence nurses (WOCNs) teach you how to change bags, prevent leaks, and care for your skin. Most patients need 3-5 sessions before feeling confident.
Permanent ostomies are often chosen for older patients (over 65), those with poor sphincter control, or those who don’t want the risks of J-pouch complications. Five-year satisfaction rates for permanent ostomy patients are 85%, according to Crohn’s & Colitis UK.
Who Gets Which Surgery?
There’s no one-size-fits-all. Surgeons match the procedure to your body and lifestyle.
- Ulcerative colitis patients under 65 with good anal function: J-pouch is the first choice. About 85% of surgeons recommend it.
- Ulcerative colitis patients over 70 or with damaged sphincters: Permanent ileostomy is safer and simpler.
- Crohn’s disease patients with localized disease: Segmental resection with primary anastomosis. But if Crohn’s returns after a J-pouch, it can destroy the pouch-so surgeons avoid it unless absolutely necessary.
- Crohn’s with multiple strictures: Strictureplasty-widening narrowed bowel without removing it-can delay or even prevent resection.
Some things rule out a J-pouch completely: severe anal damage, male impotence risk (15-20% after surgery), or female infertility (risk jumps from 15% to 50-70%). These aren’t just side effects-they’re real trade-offs.

What Happens After Surgery?
Recovery isn’t just about healing the incision. It’s about relearning how your body works.
First 2-7 days: You’re in the hospital. Pain is managed with non-opioid options when possible-IBD patients have a 22% higher risk of chronic opioid use after abdominal surgery than others. You’ll start drinking clear liquids, then move to soft foods.
Weeks 1-6: At home, you’ll focus on hydration. You need 8-10 cups of fluid daily, especially with an ileostomy. Too little can lead to dehydration and hospital readmission. Many patients are readmitted in the first 90 days for this reason.
Months 3-12: Your body adapts. J-pouch users may have 6-10 bowel movements a day at first. That drops to 4-8. You’ll learn which foods cause gas, bloating, or loose stools. High-fiber foods like raw veggies, nuts, and popcorn are often avoided early on. You’ll also learn to recognize warning signs: fever over 101°F, output over 1,500 mL per day, or sudden abdominal pain.
Support matters. The United Ostomy Associations of America and online groups like Ileostomates on Reddit offer real advice from people who’ve been there. One common tip: invest in a good ostomy belt. The Convatec Adapt Mini Belt costs about $46 and helps keep your bag secure during movement.
The Future of IBD Surgery
Surgery isn’t standing still. Robotic-assisted J-pouch procedures are becoming more common. Mayo Clinic reports 20% shorter surgery times and 15% fewer complications with robotics compared to traditional laparoscopic methods.
New tech is helping too. In 2023, the FDA approved the OstoLert smart ostomy bag by ConvaTec. It has sensors that detect leaks and send alerts to your phone. It costs $80-but for many, it’s worth it.
Researchers are also exploring microbiome transplants to prevent pouchitis. A National Institutes of Health trial showed a 40% drop in pouchitis after fecal transplants. And 3D modeling is being tested to create custom-shaped pouches that fit each patient’s anatomy better.
Still, the core truth hasn’t changed: surgery for IBD isn’t about fixing a broken organ. It’s about giving you back control of your life.
Real Outcomes, Real Lives
On the Crohn’s & Colitis Foundation’s patient forum, 78% of J-pouch patients said their quality of life improved significantly after surgery. They talked about being able to travel, sleep through the night, or play with their kids without panic.
But they also warned: don’t rush. Take time to learn. Talk to your WOCN before surgery. Join a support group. Ask about long-term risks. And remember-your surgery isn’t the end. It’s the start of a new chapter.
Is IBD surgery always permanent?
No. Many IBD surgeries involve temporary ostomies, especially when a J-pouch is built. The stoma is usually reversed after 8-12 weeks once the new connection heals. Permanent ostomies are only needed when the rectum is removed and no internal reservoir is created-or if complications make reversal unsafe.
Can you have a J-pouch if you have Crohn’s disease?
It’s rare and generally not recommended. Crohn’s can return in the J-pouch, leading to inflammation, strictures, or fistulas. Studies show up to 50% of Crohn’s patients who get a J-pouch develop recurrent disease in the pouch, and about 10% end up needing a permanent stoma. J-pouches are primarily for ulcerative colitis patients.
How long does it take to recover from J-pouch surgery?
Full recovery takes 6-12 months. The first hospital stay is 5-7 days after the colectomy. After the pouch is built, another 4-6 days in the hospital. Reversing the stoma adds another 3-5 days. But your body continues adjusting for months. Bowel frequency drops from 6-10 movements a day to 4-8 as your pouch adapts. Patience and follow-up care are key.
What are the biggest risks of J-pouch surgery?
The biggest risks are anastomotic leaks (5-15%), pouchitis (up to 40%), and infertility or sexual dysfunction. Leaks can lead to serious infections. Pouchitis requires long-term antibiotics. Women may lose fertility; men may develop erectile dysfunction. These aren’t common side effects-they’re well-documented trade-offs that need to be discussed before surgery.
Do I need special training for an ostomy?
Yes. You need training from a certified wound, ostomy, and continence nurse (WOCN). They’ll teach you how to measure your stoma, choose the right bag, prevent skin irritation, and handle leaks. Most patients need 3-5 sessions before feeling confident. Skipping this step increases the risk of complications and hospital visits.
Can I still exercise or travel after IBD surgery?
Absolutely. Most people return to normal activity within 3-6 months. Travel is easier with an ostomy-no more searching for bathrooms. Many use discreet, low-profile bags and carry extra supplies. J-pouch patients often find they can hike, swim, and even run again. The key is preparation: know your limits, stay hydrated, and carry emergency supplies.
Are there new technologies that help with ostomy care?
Yes. The FDA approved the OstoLert smart ostomy bag in 2023-it detects leaks and alerts your phone. There are also new skin barriers with longer wear times and more breathable materials. Ostomy belts have improved too, with adjustable, low-profile designs that work under clothing. These aren’t just gadgets-they’re tools that reduce anxiety and improve daily life.
What’s the difference between a temporary and permanent ileostomy?
A temporary ileostomy is created to protect a surgical connection, like a J-pouch. It’s reversed after 8-12 weeks. A permanent ileostomy means the rectum and colon are gone, and waste will always exit through the stoma. There’s no reversal. Permanent ostomies are often chosen for older patients or those with poor sphincter control to avoid the risks of pouch complications.
Does surgery cure ulcerative colitis?
Yes. Removing the entire colon and rectum cures ulcerative colitis because the disease only affects those organs. Even if you have a J-pouch, the disease won’t return. That’s why it’s the only definitive treatment. The only risk is complications from the surgery itself-not a recurrence of UC.
How do I know if I’m a good candidate for J-pouch surgery?
You’re a good candidate if you have ulcerative colitis, your anal sphincter works well, you’re under 70, and you’re in good overall health. You should be willing to accept the risks-like pouchitis or infertility-and commit to long-term follow-up. If you have Crohn’s disease, severe obesity, or prior pelvic radiation, you’re likely not a candidate.

Jaspreet Kaur
November 27, 2025 AT 06:44It's about building something new
Some days you'll hate the bag
Other days you'll thank it for letting you sleep through the night
It's not perfect
But it's freedom
Gina Banh
November 29, 2025 AT 00:59Dan Rua
November 30, 2025 AT 11:20WOCN training saved me. Don't skip it.
Mqondisi Gumede
December 2, 2025 AT 03:27Back home we just deal with it
Medicines work fine if you stop whining
They make you think you need a robot to live
Douglas Fisher
December 2, 2025 AT 11:45vikas kumar
December 2, 2025 AT 13:49Vanessa Carpenter
December 3, 2025 AT 10:13Bea Rose
December 3, 2025 AT 11:23Michael Collier
December 3, 2025 AT 22:57Deirdre Wilson
December 5, 2025 AT 06:03Damon Stangherlin
December 6, 2025 AT 11:35Ryan C
December 7, 2025 AT 09:20Albert Guasch
December 8, 2025 AT 18:22Ginger Henderson
December 9, 2025 AT 21:28