How Thyroid Disorders Affect Your Bones: Causes, Risks, and Prevention
Thyroid & Bone Health Risk Calculator
This tool helps assess your risk of developing bone-related complications due to thyroid disorders. Answer the following questions based on your current situation.
Recommendation:
When you hear thyroid disorders are conditions that affect how the thyroid gland makes hormones, influencing metabolism, heart rate, and body temperature, you probably think of weight changes or fatigue. What most people miss is that the same hormonal imbalance can quietly sabotage the strength of your skeleton. Below we break down why the thyroid and bones are tightly linked, what signs to watch for, and simple steps to keep both systems running smoothly.
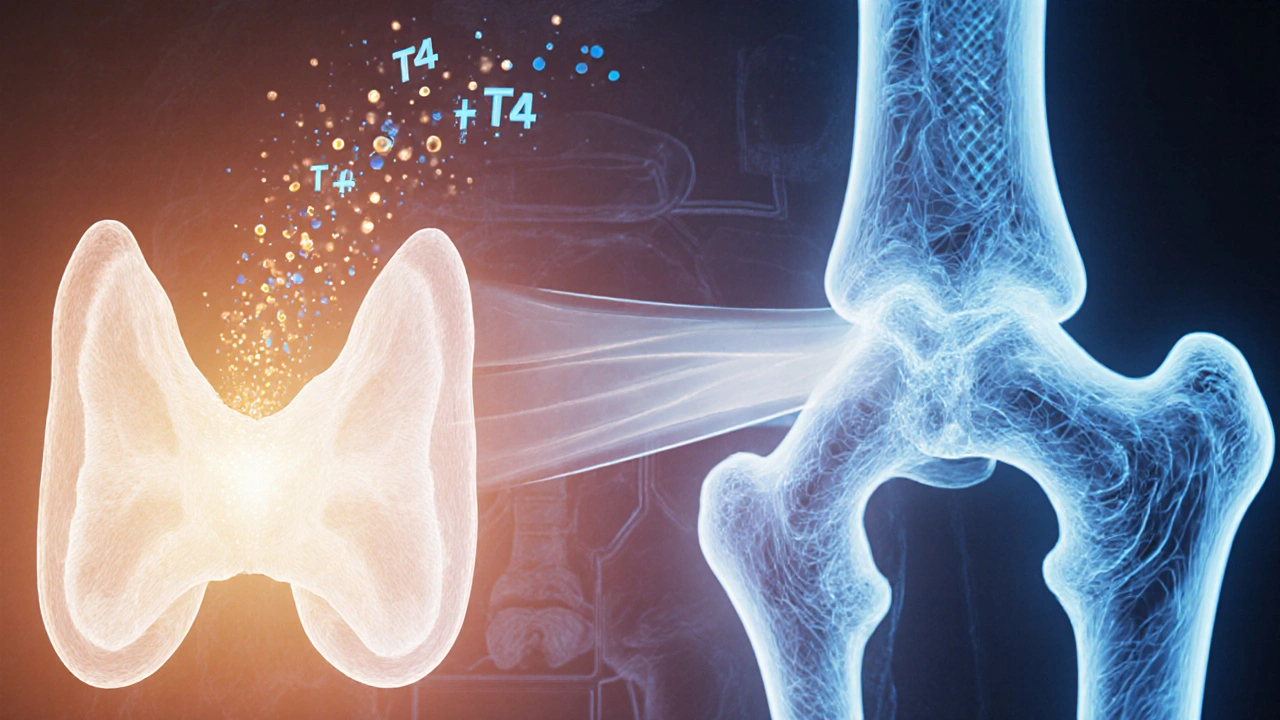
Why the Thyroid Matters for Your Skeleton
The thyroid releases two key hormones - thyroxine (T4) and triiodothyronine (T3). These hormones tell almost every cell in your body how fast to work. When their levels are too high (hyperthyroidism) or too low (hypothyroidism), bone turnover goes off‑track.
- In hyperthyroidism, the bone‑removing cells called osteoclasts break down bone tissue as part of normal remodeling become over‑active, leading to faster loss of bone mass.
- In hypothyroidism, the opposite happens - bone‑building slows down, but the body also loses the ability to absorb crucial minerals like calcium the primary mineral that gives bone its hardness, leaving you with weaker bones over time.
Both extremes raise the risk of osteoporosis a condition where bones become porous and fracture‑prone, even if you’re young and active.
Key Players in the Thyroid‑Bone Connection
Understanding the chain of events helps you see where you can intervene.
| Factor | How it affects bone | Typical level in disorder |
|---|---|---|
| Thyroid hormones (T3/T4) | Regulate bone remodeling speed | High in hyper, low in hypo |
| Parathyroid hormone (PTH) | Controls calcium release from bone | May rise to compensate for low calcium |
| Vitamin D | Facilitates calcium absorption in gut | Often deficient when thyroid meds interfere with metabolism |
| Bone density test | Measures mineral content, flags early loss | Recommended annually for high‑risk thyroid patients |
These pieces fit together like a puzzle: hormone imbalance → altered PTH & Vitamin D balance → calcium mishandling → bone loss.
Symptoms That Might Hint at Bone Damage
Bone problems develop silently, but a few clues can alert you.
- Sudden back or hip pain after a minor fall.
- Loss of height or a noticeable stooped posture.
- Frequent fractures of the wrist, ankle, or ribs.
- Persistent muscle weakness that feels unrelated to thyroid fatigue.
If any of these show up alongside thyroid symptoms, it’s time to ask your doctor for a bone density test.
How Medications Influence Bone Health
Medication can be a double‑edged sword.
- Levothyroxine (synthetic T4) - When dose is too high, it mimics hyperthyroidism, speeding up bone loss.
- Antithyroid drugs (e.g., methimazole) - Over‑suppression may lead to low bone turnover, making bone less able to repair micro‑damage.
- Radioactive iodine therapy - Can trigger a temporary dip in thyroid hormone, sometimes worsening calcium balance.
Regular blood tests to keep hormone levels in the target range are essential. If you’re on long‑term therapy, ask your clinician about a yearly bone density test and consider calcium/vitamin D supplements.
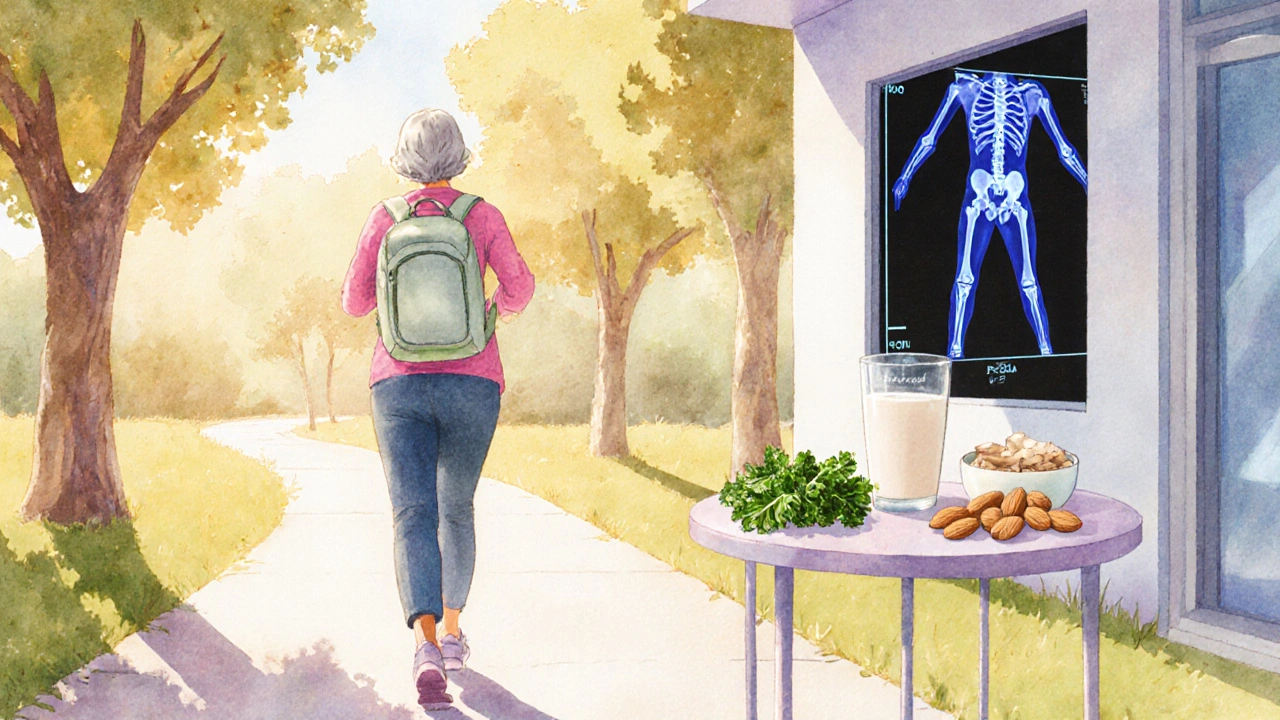
Practical Ways to Protect Your Bones
Here’s a roadmap you can start today.
- Get your calcium intake right: Aim for 1,000mg/day (1,200mg if you’re over 50). Dairy, fortified plant milks, leafy greens, and almonds are good sources.
- Boost vitamin D: 800-1,000 IU daily works for most adults; sunlight for 10-15minutes a few times a week helps too.
- Exercise smart: Weight‑bearing activities - brisk walking, jogging, resistance training - signal bones to stay strong.
- Watch your medication dose: Keep thyroid hormone levels within the normal lab range; don’t self‑adjust.
- Stay on top of screenings: A bone density scan (DEXA) every 1-2years if you have a thyroid disorder, especially post‑menopausal women.
- Limit caffeine & alcohol: Excessive intake can increase calcium loss.
These habits work whether you have hyper‑ or hypothyroidism; they just become more critical when the thyroid is out of whack.
When to Seek Professional Help
If you notice any of the warning signs listed earlier, or if your thyroid medication has been tweaked recently, schedule an appointment. A typical work‑up includes:
- Blood panel - TSH, free T4, free T3, calcium, vitamin D, and PTH.
- Bone density scan - DEXA or quantitative CT.
- Review of diet & exercise - Your doctor may refer you to a dietitian or physiotherapist.
Early detection can mean the difference between a reversible bone loss and a permanent fracture risk.
Bottom Line
The thyroid and skeleton are in constant conversation. When that dialogue gets garbled, your bones pay the price. By keeping hormone levels stable, feeding your body the right minerals, and checking bone health regularly, you can protect yourself from the hidden danger of bone damage.
Frequently Asked Questions
Can hypothyroidism cause osteoporosis?
Yes. Low thyroid hormone slows bone remodeling, which can reduce calcium absorption and lead to lower bone density over time.
Does taking levothyroxine increase fracture risk?
If the dose is too high, it mimics hyperthyroidism and can accelerate bone loss, raising fracture risk. Proper dosing mitigates this.
What’s the best calcium source for someone with thyroid disease?
Dairy products, fortified soy or almond milk, and low‑oxalate leafy greens (like kale) provide calcium without interfering with thyroid medication absorption.
How often should I get a DEXA scan if I have a thyroid disorder?
Most specialists recommend every 1‑2years for adults over 40 with thyroid disease, or sooner if you have other risk factors like early menopause.
Can vitamin D supplements help protect my bones while on thyroid medication?
Adequate vitamin D (800‑1,000IU daily) improves calcium absorption and has been shown to reduce bone loss in both hyper‑ and hypothyroid patients.

Nancy Chen
October 10, 2025 AT 20:56Ever notice how every new ``thyroid‑bone'' article seems to pop up right after a pharma press release? It's like they're hiding the fact that the big players are tweaking calcium guidelines to keep us dependent on pricey supplements. The calculator looks slick, but I bet the real algorithm is hidden behind a firewall of corporate interests. Stay alert, folks-your bones might be paying the price for someone else's profit.
Jon Shematek
October 18, 2025 AT 03:59Hey, don’t let the scary headlines get you down! If you’ve got a thyroid issue, just follow the simple steps: get your vitamin D levels checked, keep moving, and talk to your doc about the right meds. You’ve got this, and the calculator is a great start to taking control of your bone health.
Josephine Bonaparte
October 25, 2025 AT 11:03Okay, a quick grammar tip while we’re at it: when you write "thyroid disorders" it’s plural, so don’t add an extra "s" after "disorder". Also, "bone‑density" should have a hyphen. Small details, big impact-just like getting enough calcium can make a huge difference in bone strength! Keep those sentences tight and your calcium intake higher.
Meghan Cardwell
November 1, 2025 AT 17:06From a clinical perspective, the interplay between TSH suppression and osteoclast activation is a key pathophysiological axis. When the thyroid is overactive, you see increased bone turnover markers, which can accelerate microarchitectural deterioration. Ensuring adequate calcium, vitamin D, and possibly bisphosphonate therapy in high‑risk patients can mitigate this cascade. The risk calculator is essentially quantifying that cascade in a user‑friendly format.
stephen henson
November 9, 2025 AT 00:10👍 Stay consistent with your supplement schedule.
Mildred Farfán
November 16, 2025 AT 07:13Oh great, another "interactive tool" that magically tells you how to fix your bones. Because we all have a personal endocrinologist on standby, right? Honestly, if you follow the basic advice-sun, dairy, and a doc visit-you're probably fine. No need for a flashy calculator to tell you what common sense already knows.
Danielle Flemming
November 23, 2025 AT 14:17Love seeing tools that actually give you a clear picture! If your score lands in the moderate‑risk zone, crank up those calcium‑rich foods and grab a quick walk outside. You’ll be surprised how small tweaks can add up to stronger bones over time.
Erynn Rhode
November 30, 2025 AT 21:20Let’s unpack this a bit: the calculator asks about dairy intake, which is great because calcium is a cornerstone of bone mineralization; however, you also need vitamin D to facilitate calcium absorption, so sunshine or supplementation is essential. Additionally, the bone density test (DEXA) provides a baseline that can guide therapeutic decisions-especially for those on levothyroxine, as overtreatment can increase bone resorption. Finally, age over 50 adds another layer of risk due to natural hormonal changes. So, while the tool is simple, it captures several critical variables that together paint a comprehensive risk profile. Keep track of your answers, discuss them with your physician, and consider a repeat DEXA every few years if you’re in a higher risk bracket.
Rhys Black
December 8, 2025 AT 04:24You really think plugging a few checkboxes will absolve you from the moral responsibility of maintaining your health? It’s absurd to rely on a calculator when you could be engaging in real, disciplined lifestyle choices. The world needs fewer shortcuts and more accountability.
Abhishek A Mishra
December 15, 2025 AT 11:27Yo, Jon’s optimism is spot on-just add a daily walk and some milk, and you’re golden. The tool is a neat way to see where you stand, but the real work is in the kitchen and the gym.
Jaylynn Bachant
December 22, 2025 AT 18:31Isn't it fascinating how our bodies are tiny universes, each hormone a star influencing the constellations of our health? When the thyroid whispers too loudly, the bones hear a different story, one of subtle erosion. Yet, like any philosophical paradox, understanding the balance can lead us to a deeper appreciation of our own fragility and strength.
Anuj Ariyo
December 30, 2025 AT 01:34Alright, let’s dive deep. First, the thyroid produces hormones that regulate metabolism, which directly influences bone remodeling cycles. When you have hyperthyroidism, the increased metabolic rate accelerates bone turnover, meaning osteoclasts break down bone faster than osteoblasts can rebuild it. Over time, this imbalance leads to decreased bone mineral density, making fractures more likely. Second, medication matters: levothyroxine, while essential for hypothyroid patients, can cause subclinical hyperthyroidism if dosed too high, replicating the same effect on bone resorption. Third, calcium intake is non‑negotiable; without sufficient dietary calcium, the body will leach calcium from the bone matrix to maintain serum levels. Fourth, vitamin D acts as the gatekeeper for calcium absorption; deficiency here compounds the problem. Fifth, sun exposure provides natural vitamin D synthesis, which is especially vital for those living in higher latitudes or who spend most time indoors. Sixth, age is a critical modifier-post‑menopausal women experience estrogen loss, which already predisposes them to osteoporosis, and any thyroid imbalance can exacerbate this. Seventh, DEXA scans give an objective measurement of bone density, allowing clinicians to stratify risk and intervene early. Eighth, lifestyle factors such as smoking and excessive alcohol use further degrade bone quality. Ninth, weight‑bearing exercise stimulates osteoblast activity, counteracting the catabolic effects of excess thyroid hormone. Tenth, regular monitoring of TSH levels ensures you stay within the therapeutic window, reducing the risk of over‑suppression. Eleventh, nutrition beyond calcium-magnesium, phosphorus, and vitamin K2-all play supportive roles. Twelfth, certain foods like cruciferous vegetables can interfere with thyroid hormone synthesis if consumed in massive amounts, but moderation is key. Thirteenth, stress management is important because cortisol can also affect bone metabolism. Fourteenth, genetics set a baseline; some people are naturally more resilient, others not. Fifteenth, staying hydrated aids overall metabolic processes, including bone health. Finally, the calculator you mentioned is a useful snapshot, but it’s your day‑to‑day choices that write the real story of your skeletal resilience.
Tom Lane
January 6, 2026 AT 08:38Great breakdown, Anuj! I’d add that incorporating short, high‑intensity interval training can boost bone density even more effectively than steady‑state cardio. Keep monitoring those labs and stay proactive.
Darlene Young
January 13, 2026 AT 15:42Danielle’s energy is contagious! If you’re scoring moderate‑risk, think about adding fortified plant milks if dairy isn’t your thing-almond, soy, or oat can boost calcium without the extra saturated fat.
Steve Kazandjian
January 20, 2026 AT 22:45Also, don’t forget about greens like kale and bok choy; they’re calcium‑rich and give you a veggie boost.
Roger Münger
January 28, 2026 AT 05:49While both suggestions are valid, it is essential to quantify calcium intake against the Recommended Dietary Allowance (RDA) of 1,000–1,200 mg per day for adults over 50, and to verify serum 25‑hydroxyvitamin D levels to ensure optimal absorption.
Gerald Bangero
February 4, 2026 AT 12:52Take away the fear, Nancy-just keep an eye on your labs, get that sunshine, and enjoy a balanced diet. Your bones will thank you.