How Stomach Ulcers Are Linked to Helicobacter pylori Infection
H. pylori Risk Assessment Tool
Assess Your Risk
Answer these questions to determine your risk level for Helicobacter pylori infection and stomach ulcers.
Key Takeaways
- Helicobacter pylori is the leading cause of most stomach (peptic) ulcers.
- The bacteria damages the gastric lining by producing urease and inflammation.
- Non‑invasive tests (urea breath, stool antigen) and endoscopy with biopsy confirm infection.
- Standard treatment combines two antibiotics with a proton‑pump inhibitor for 10‑14 days.
- Good hygiene, safe food handling, and avoiding unnecessary NSAIDs lower reinfection risk.
Stomach ulcer is a sore that forms on the inner lining of the stomach or the upper part of the small intestine. When the lining is eroded, acid and digestive enzymes can irritate the tissue, causing pain, bleeding, or even perforation. While many factors contribute to ulcer formation, the bacterium Helicobacter pylori-commonly called H. pylori-accounts for roughly 70 % of cases worldwide.
What Exactly Is a Stomach Ulcer?
Medically, a stomach ulcer belongs to the broader category of peptic ulcer disease (PUD). It differs from gastric erosion, which is a superficial, temporary irritation. An ulcer creates a pocket of tissue loss that can persist for weeks or months if untreated.
Typical symptoms include a gnawing or burning pain between meals, bloating, nausea, and in severe cases, vomiting blood or black stools. However, up to 30 % of individuals remain asymptomatic, which makes screening essential for high‑risk groups.
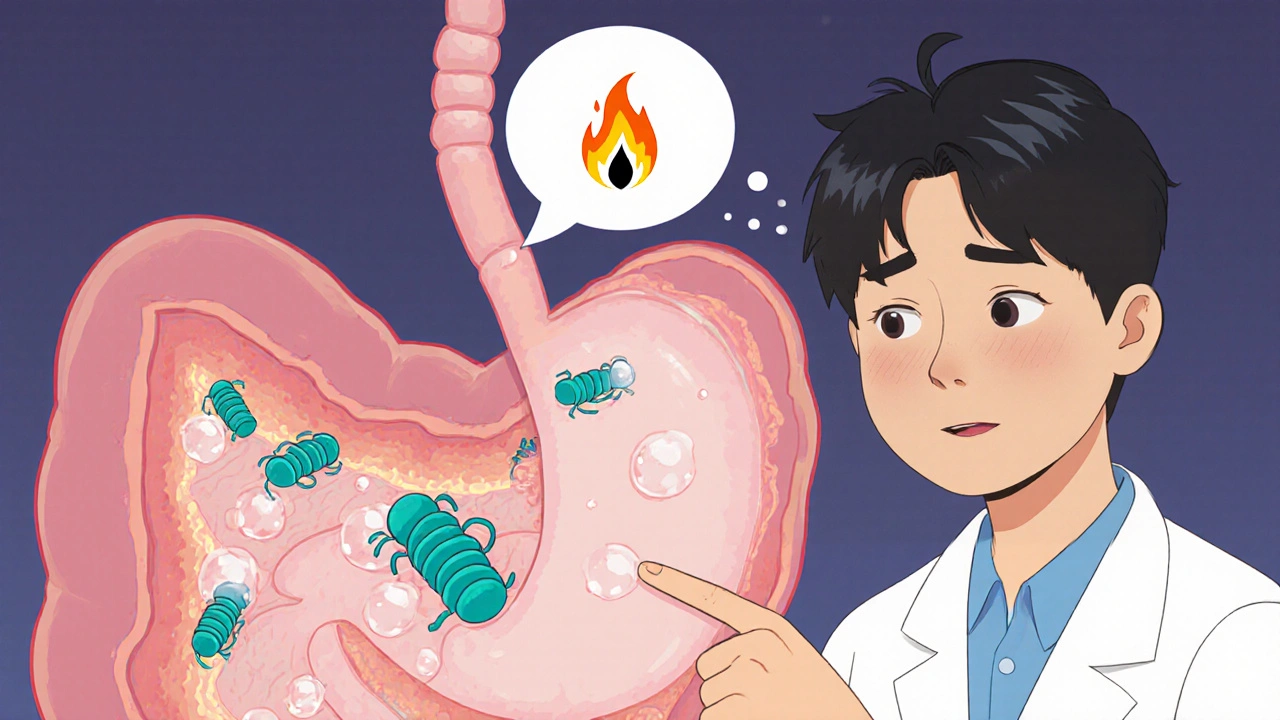
Helicobacter pylori: The Bacterial Culprit
Discovered in 1982 by Barry Marshall and Robin Warren, Helicobacter pylori is a spiral‑shaped, gram‑negative bacterium that thrives in the acidic environment of the stomach. It colonizes the gastric mucosa, the mucus‑rich protective layer lining the stomach wall.
The organism’s survival hinges on two key enzymes: urease, which converts urea into ammonia to neutralize acid, and flagella, which allow it to burrow through mucus. These adaptations let the bacterium persist for decades, often unnoticed.
How H. pylori Triggers Ulcer Formation
The ulcer‑causing process can be broken down into three overlapping steps:
- Direct mucosal damage: The bacteria’s urease activity raises local pH, weakening the mucus barrier and exposing epithelial cells to gastric acid.
- Inflammatory response: Infection stimulates immune cells to release cytokines (IL‑1β, TNF‑α). This chronic inflammation disrupts the balance between aggressive factors (acid, pepsin) and defensive factors (bicarbonate, mucus).
- Altered acid regulation: H. pylori can either increase or decrease gastric acid secretion, depending on the strain’s virulence factors (CagA, VacA). Hyper‑acidic environments accelerate tissue erosion, while hypo‑acidic states favor bacterial overgrowth.
Combined, these mechanisms create a perfect storm for ulcer development.
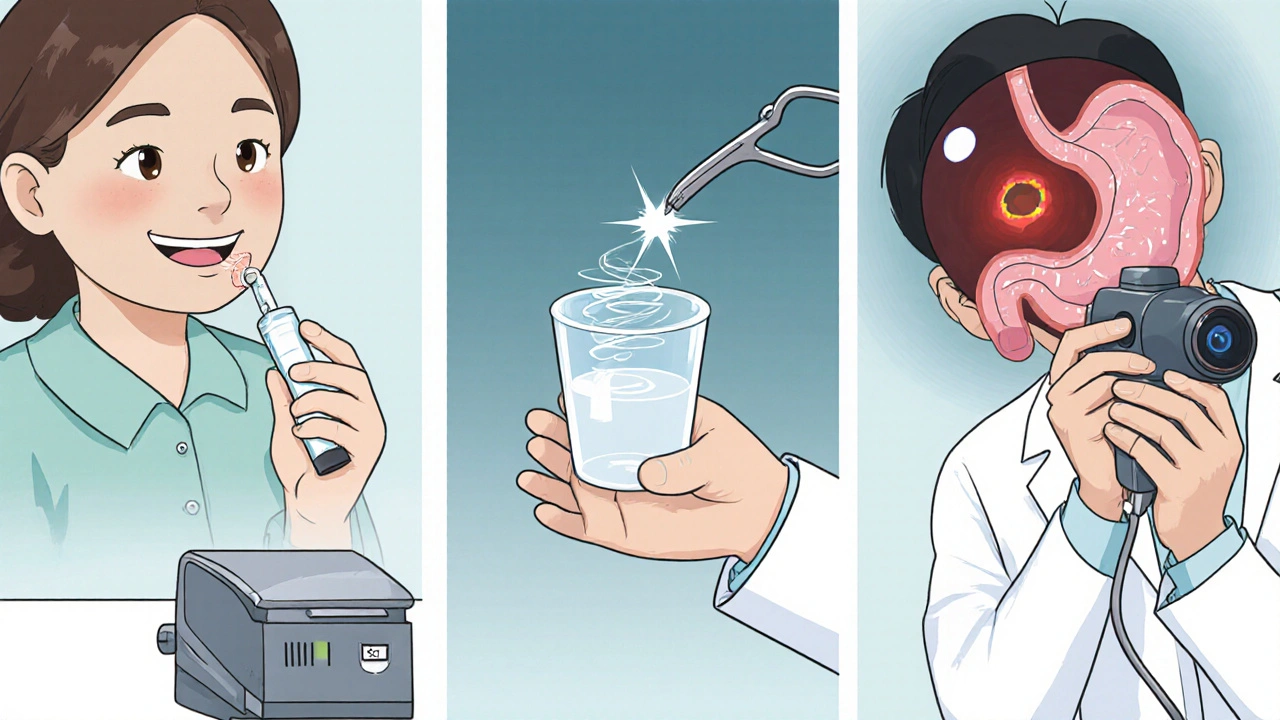
Diagnosing H. pylori‑Related Ulcers
Accurate diagnosis guides treatment. Physicians choose among invasive and non‑invasive methods based on symptom severity, patient age, and local resource availability.
| Test | Invasiveness | Accuracy | Typical Use |
|---|---|---|---|
| Urea Breath Test | Non‑invasive | 90‑95 % | Initial screening, post‑treatment check |
| Stool Antigen Test | Non‑invasive | 85‑90 % | Children, low‑resource settings |
| Serology (blood antibody) | Non‑invasive | 70‑80 % | Epidemiological surveys |
| Endoscopy with Biopsy | Invasive | 95‑99 % | Severe symptoms, suspicion of cancer |
After confirming infection, an upper‑GI endoscopy visualizes the ulcer, takes biopsies for histology, and rules out malignancy.
Standard Treatment Regimens
Since the early 1990s, the accepted cure-often called “triple therapy”-combines two antibiotics with a proton‑pump inhibitor (PPI) to suppress acid and enhance bacterial eradication.
- Antibiotics: Common pairs include clarithromycin + amoxicillin or metronidazole + amoxicillin.
- PPI: Omeprazole, esomeprazole, or lansoprazole taken twice daily.
- Duration: 10‑14 days, depending on local resistance patterns.
If resistance to clarithromycin exceeds 15 % in a region, clinicians often opt for “concomitant therapy” (adding a fourth drug, usually a nitroimidazole) or “bismuth quadruple therapy” (bismuth subsalicylate, metronidazole, tetracycline, and a PPI).
Follow‑up testing-usually a urea breath test-occurs 4‑6 weeks after therapy to confirm eradication.
Managing Ulcer Symptoms While Treating Infection
Acid‑suppressing agents help the ulcer heal faster. H2 blockers (e.g., ranitidine) are less potent than PPIs but may be used for maintenance after eradication. Additionally, protective agents like sucralfate can coat the ulcer base, reducing pain.
Patients are advised to avoid NSAIDs, smoking, and excessive alcohol, all of which impede healing and increase recurrence risk.

Prevention and Lifestyle Tips
Because H. pylori spreads through contaminated food, water, and close personal contact, simple hygiene cuts transmission:
- Wash hands with soap after using the restroom and before meals.
- Consume water that’s been boiled or filtered.
- Eat foods prepared at reputable establishments; avoid raw, unpasteurized dairy in high‑risk areas.
- Limit use of over‑the‑counter antacids unless prescribed.
Family members of an infected individual should be screened, especially in regions where infection rates exceed 50 %.
What to Expect After Treatment
Most patients experience symptom relief within a week, but complete ulcer healing on endoscopy can take 4‑8 weeks. Regular follow‑up appointments help monitor for complications such as bleeding or perforation, which, although rare, require emergency care.
Frequently Asked Questions
Can a stomach ulcer heal without treating H. pylori?
Spontaneous healing is uncommon. Without eradication, the bacterium continues to damage the mucosa, leading to recurrence or complications.
Is H. pylori infection always harmful?
About 30‑40 % of infected people never develop ulcers or cancer. The bacterium can coexist harmlessly, but risk rises with certain virulence factors and lifestyle habits.
How long does the eradication test wait after therapy?
Four to six weeks is standard to avoid false‑negative results caused by residual antibiotics.
Can I use probiotics during treatment?
Probiotics such as Lactobacillus or Bifidobacterium may reduce antibiotic‑associated side effects, but they should complement-not replace-prescribed therapy.
What are the signs of a serious ulcer complication?
Sudden, severe abdominal pain, vomiting blood, or black/tarry stools indicate possible bleeding or perforation and require immediate medical attention.
Understanding the link between Helicobacter pylori and stomach ulcers empowers you to seek the right tests, complete the correct treatment, and adopt habits that keep the infection at bay.

ashanti barrett
October 18, 2025 AT 21:56Take the infection seriously, because untreated H. pylori can silently damage the stomach lining.
Leo Chan
October 26, 2025 AT 16:08Staying positive during the triple‑therapy phase really helps you push through the side effects; remember that most people feel better within a week.
jagdish soni
November 3, 2025 AT 11:20When you look beyond the biochemical cascade you see a narrative of survival and subversion.
The spiral bacterium fashions its own micro‑world in the harsh acidic sea of the stomach.
Its urease enzyme fashions a pocket of ammonia that neutralizes the surrounding acid.
This localized pH shift strips away the protective mucus barrier.
Exposed epithelial cells then meet an onslaught of gastric acid and pepsin.
The immune system answers with cytokines that inflame the tissue.
Chronic inflammation tilts the balance toward erosion rather than repair.
Certain strains carry CagA and VacA which further manipulate host signaling.
The result is a perfect storm that gnaws at the mucosa.
Ulcers that emerge can linger for months if left unchecked.
Diagnostic breath tests capture the lingering metabolic fingerprint of urease activity.
Endoscopic biopsies reveal the bacterial colonies amid the damaged tissue.
Treatment combines two antibiotics with a proton‑pump inhibitor to starve the bug and calm the acid.
Adherence to the full course is crucial; resistance thrives on half‑measures.
After eradication, the mucosa begins a slow healing process that may take weeks.
Latasha Becker
November 11, 2025 AT 06:32The pathophysiology you described aligns with the canonical model of H. pylori‑induced mucosal disruption, specifically via urease‑mediated ammonia production and subsequent cytokine‑driven inflammatory cascades; consequently, the acid–base equilibrium is perturbed, precipitating epithelial apoptosis and ulcerogenesis.
parth gajjar
November 19, 2025 AT 01:44What a melodramatic recount of bacteria playing god over our stomachs it feels like a tragedy in microscopic form
Maridel Frey
November 26, 2025 AT 20:56For anyone embarking on eradication therapy, it is advisable to schedule a follow‑up urea breath test four weeks post‑treatment to confirm bacterial clearance; this step ensures that residual infection does not precipitate recurrence.
Madhav Dasari
December 4, 2025 AT 16:08Also, don’t forget to hydrate well and maybe add a probiotic yogurt to your diet – it can soothe the gut while the antibiotics do their job.
DHARMENDER BHATHAVAR
December 12, 2025 AT 11:20Urease breath testing is non‑invasive and boasts over 90 % accuracy.
Kevin Sheehan
December 20, 2025 AT 06:32The battle against H. pylori is more than a medical regimen it is a struggle between microscopic opportunism and human agency; we wield antibiotics like swords and PPIs like shields; surrender is not an option.
Jay Kay
December 28, 2025 AT 01:44Skipping the triple therapy is like ignoring a fire alarm – you’ll soon be overwhelmed by the blaze.
Jameson The Owl
January 4, 2026 AT 20:56The mainstream medical narrative tells us that H. pylori is simply a common pathogen far too benign to warrant suspicion.
What they hide is the coordinated effort of global health agencies to downplay the true prevalence of resistant strains.
Every prescription of clarithromycin is a step toward a silent antibiotic arms race.
The data from independent labs show resistance rates soaring well beyond the cited 15 percent.
Meanwhile the pharmaceutical lobby pushes new proton pump inhibitors as a panacea.
They ignore the fact that long term acid suppression can alter gut flora in ways that promote other diseases.
The ideal solution is to return to rigorous hygiene protocols rather than rely on chemical suppression.
Boil your water, wash your produce, and demand transparent testing for every batch of antibiotics.
If you walk into a clinic and ask about strain typing you will be met with canned responses.
The truth is buried beneath layers of regulatory red tape designed to protect profit margins.
Communities with high infection rates are often the ones denied access to proper diagnostic tools.
This creates a feedback loop where the disease spreads unchecked while official statistics remain artificially low.
The only way to break this cycle is collective awareness and refusal to accept half‑truths.
Share reliable resources, support open‑source research, and challenge any authority that dismisses your concerns.
In the end the battle is not just against a bacterium but against a system built on complacency.