Gallbladder and Biliary Disease: Understanding Stones, Cholangitis, and ERCP

When your gallbladder stops working right, the pain doesn’t just come and go-it hits like a freight train. Imagine a dull ache under your right ribs that suddenly explodes into sharp, unrelenting pain, lasting hours, often after a fatty meal. You might feel nauseous, sweaty, or notice your skin turning yellow. This isn’t just indigestion. It’s your bile system screaming for help. Gallbladder and biliary diseases are more common than most people realize, affecting gallbladder stones in 1 in 6 adults in the U.S., especially women over 40. The real danger isn’t the stones themselves-it’s what happens when they block the ducts. That’s where cholangitis and ERCP come in.
What Are Gallstones, Really?
Gallstones aren’t just hard lumps. They’re crystallized chunks of bile-mostly cholesterol or bilirubin-that form inside the gallbladder. About 80% are cholesterol stones, the kind that build up when your liver dumps too much cholesterol into bile and your gallbladder doesn’t empty properly. The other 20% are pigment stones, made of bilirubin, often linked to liver disease, blood disorders, or even genetics. In Asian populations, pigment stones are far more common than in Western countries.
Here’s the twist: most people with gallstones never know they have them. Around 80% of cases are silent. You could live your whole life with them and never need treatment. But if one gets stuck-especially in the cystic duct (the tube leading out of the gallbladder)-it triggers inflammation. That’s acute cholecystitis. Pain spikes, fever kicks in, and you’re headed to the ER. Ultrasound is the first test. It catches gallstones with 96% accuracy and is quick, safe, and non-invasive.
When Stones Move: Cholangitis and the Danger Zone
Not all blockages are created equal. If a stone slips from the gallbladder into the common bile duct, it’s a whole different problem. That duct carries bile from the liver to the intestine. Block it, and bile backs up. Bacteria grow. Infection spreads. That’s cholangitis-and it’s dangerous.
The classic signs? Charcot’s triad: right upper abdominal pain, fever, and jaundice (yellow skin or eyes). If you add low blood pressure or confusion, you’ve moved into Reynolds’ pentad. That means sepsis is coming. This isn’t a wait-and-see situation. Cholangitis can kill within hours if untreated. It’s why doctors don’t wait when someone with gallstones shows these signs.
Why does this happen more in older adults? Because bile flow slows with age, and stones get bigger. Women are more affected-partly due to hormones, partly because they’re more likely to have cholesterol-rich bile. Obesity, rapid weight loss, diabetes, and cirrhosis all raise your risk. Native American populations, especially Pima Indians, have the highest rates globally-up to 64% in some groups.
ERCP: The Lifesaving Procedure That’s Also Risky
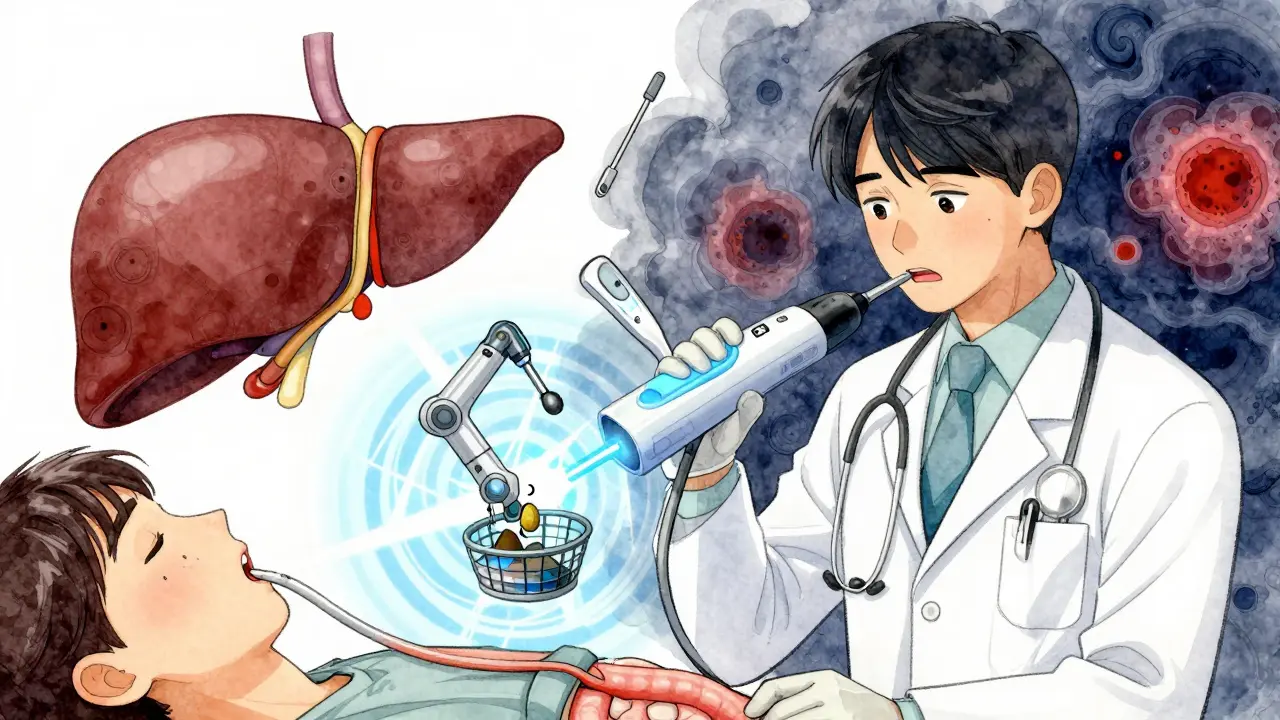
So how do you get a stone out of a bile duct without cutting open the abdomen? Enter ERCP-Endoscopic Retrograde Cholangiopancreatography. It’s not a surgery. It’s a procedure done through your mouth.
A thin, flexible scope is passed down your throat, through your stomach, and into the small intestine. At the ampulla of Vater (where the bile duct opens), the doctor injects dye and takes X-rays to find the stone. Then, using tiny tools, they cut the muscle around the duct (sphincterotomy), grab the stone with a basket, and pull it out. Success rates? Over 90% in experienced hands.
But here’s the catch: ERCP isn’t perfect. About 3-10% of patients develop post-ERCP pancreatitis-sometimes severe. It’s the most common complication. Why? Because the tools can irritate the pancreatic duct, which sits right next to the bile duct. Patients with Sphincter of Oddi dysfunction are at higher risk. That’s why ERCP shouldn’t be used just to look. If you don’t need to remove something, don’t do it. MRCP (Magnetic Resonance Cholangiopancreatography) is the better first step. It’s an MRI of the bile ducts-no cutting, no radiation, 95% accurate. Use it to confirm the stone. Then use ERCP to remove it.
And yes, the equipment matters. In 2023, the FDA approved new duodenoscopes with disposable parts. Why? Because old designs caused outbreaks of deadly superbugs. Between 2013 and 2018, 112 infections were traced back to contaminated scopes. Modern devices cut that risk dramatically.
What About Removing the Gallbladder?
If you’ve had one attack, your chance of another is 70% within 10 years. That’s why most doctors recommend removing the gallbladder-cholecystectomy-after a first symptomatic episode. The gold standard? Laparoscopic surgery. Four tiny cuts, a camera, and tools. You’re usually home the next day. Recovery? About a week. Open surgery? That’s for emergencies or complex cases. Hospital stay: 5 days. Recovery: 6 weeks.
But here’s the problem: too many people get their gallbladder removed for no reason. About 20% of the 600,000 cholecystectomies done each year in the U.S. are for people with mild or no symptoms. Guidelines say: if you’re not in pain, leave it alone. The risk of complications from surgery outweighs the 1-2% annual risk of developing symptoms.
And after removal? About 12% of people still have pain-called post-cholecystectomy syndrome. Some get diarrhea because bile flows straight into the intestine instead of being stored. It’s not rare. Loperamide helps. Most people adapt within 6 weeks. But for some, it lasts months.
Medical Treatments: Do They Work?
Some people hope for a pill to dissolve stones. Ursodeoxycholic acid (UDCA) can work-for small cholesterol stones under 15mm. But it takes 6-12 months. And only 30-40% of stones dissolve. Plus, they often come back within 5 years. It’s not worth it for most. It’s useless for pigment stones.
Shock wave therapy? Used to be popular. Now it’s nearly abandoned. It breaks stones, but they often stay in the duct. You still need ERCP. And recurrence rates are high. Not worth the hassle.
Right now, there’s no good drug for pigment stones. Researchers are trying to develop new agents targeting calcium bilirubinate. That’s the holy grail. But it’s still years away.

Who Needs What? A Practical Guide
Let’s cut through the noise. Here’s what actually works in real life:
- Asymptomatic stones? Do nothing. Monitor. Don’t operate.
- One attack, clear stones on ultrasound? Plan for laparoscopic cholecystectomy. Don’t wait for the next one.
- Pain + jaundice + fever? Suspect common bile duct stone. Do MRCP first. If confirmed, do ERCP right away-ideally during the same hospital stay as your cholecystectomy. Only 30-40% of patients get this done now. That’s a waste of time, money, and risk.
- ERCP needed? Go to a high-volume center. Hospitals doing over 100 ERCPs a year have 20% fewer complications. Ask your doctor.
- After ERCP or surgery? Eat low-fat for 2-4 weeks. Most resume normal eating by 6 weeks. Watch for diarrhea. It’s common. It’s manageable.
The Bigger Picture
Gallbladder and biliary diseases cost the U.S. healthcare system $6.2 billion a year. Cholecystectomy is the 9th most common surgery. The ERCP equipment market is set to hit $1.8 billion by 2027. But money isn’t the real issue. The real issue is knowing when to act-and when not to.
Too many patients get swept into procedures they don’t need. Too many wait too long and end up in the ICU with cholangitis. The key is early, accurate diagnosis and avoiding unnecessary interventions. Ultrasound first. MRCP if needed. ERCP only to remove. Cholecystectomy only if you’ve had symptoms.
And if you’ve had your gallbladder removed and still feel off? You’re not alone. Talk to your doctor. It’s not all in your head. It’s bile flow. It’s manageable. You just need the right advice.
Can gallstones dissolve on their own without treatment?
Rarely. Most gallstones stay the same size or grow over time. Only small cholesterol stones (under 15mm) have a chance of dissolving with medication like UDCA, and even then, it takes months and only works in about one-third of cases. Most stones don’t dissolve on their own. Waiting rarely helps-it just increases the risk of complications like infection or pancreatitis.
Is ERCP dangerous?
ERCP is generally safe when done by experienced providers, but it carries risks. The most common complication is post-ERCP pancreatitis, which happens in 3-10% of cases. Other risks include bleeding, infection, or perforation. The risk goes up if you’ve had previous abdominal surgery, have Sphincter of Oddi dysfunction, or if the procedure is done at a low-volume center. Always ask how many ERCPs the doctor performs each year-high-volume centers have significantly lower complication rates.
Why do women get gallstones more often than men?
Estrogen plays a big role. Women, especially those on birth control or hormone therapy, produce more cholesterol in bile and have slower gallbladder emptying. Pregnancy also increases risk due to hormonal shifts. That’s why gallstones affect women 2.1 times more than men, and the risk climbs after age 40. Obesity and rapid weight loss add to the risk, especially in women.
Can you live without a gallbladder?
Yes, absolutely. The gallbladder stores bile, but your liver still makes it. After removal, bile flows directly into your intestine. Most people adapt well. Some get loose stools after fatty meals for a few weeks or months, but 75% return to normal eating within 6 weeks. A low-fat diet right after surgery helps ease the transition. Long-term, there’s no major impact on digestion or life expectancy.
What’s the difference between MRCP and ERCP?
MRCP is a non-invasive MRI scan that shows detailed images of your bile ducts and pancreas. It’s used to diagnose stones or blockages without any tools entering your body. ERCP is a therapeutic procedure where a scope goes through your mouth to remove stones or place stents. Think of MRCP as the camera that finds the problem. ERCP is the tool that fixes it. Always do MRCP first unless you’re in an emergency.
Should I get my gallbladder removed if I have stones but no symptoms?
No, not unless you’re in a high-risk group. Guidelines from the American College of Gastroenterology say asymptomatic gallstones don’t need surgery. The risk of developing symptoms is only 1-2% per year, and the risk of serious complications from surgery is higher than that. Exceptions include people with sickle cell disease, polycythemia, or those planning bariatric surgery. For most, watchful waiting is the best approach.
What Comes Next?
If you’ve been diagnosed with gallstones, don’t panic. Get the right tests. Ask about MRCP before ERCP. Talk to a gastroenterologist and a surgeon. Ask: "Is this necessary? Are there alternatives? What happens if I wait?"
If you’ve had surgery or ERCP and still have symptoms, keep track. Note what you eat, when the pain hits, and how long it lasts. That info helps your doctor figure out if it’s bile reflux, Sphincter of Oddi dysfunction, or something else.
And if you’re healthy? Maintain a steady weight. Avoid crash diets. Eat fiber. Stay active. These simple steps cut your risk of gallstones by half. You don’t need a miracle cure. Just smart habits.

Raushan Richardson
December 27, 2025 AT 22:19This is such a clear breakdown-I’ve had gallstones and honestly, no one ever explained it like this. I thought it was just ‘bad digestion’ until I ended up in the ER. The part about MRCP before ERCP? YES. My first doc wanted to jump straight to ERCP. I pushed back and got the MRI first. Saved me from pancreatitis. Thank you for writing this.
Liz MENDOZA
December 28, 2025 AT 10:50I’m a nurse who’s seen too many patients get scared into surgery they didn’t need. This post nails it. Asymptomatic stones = leave them alone. So many people panic and demand removal, but the risks aren’t worth it unless you’re in pain. I wish more docs followed this. Thank you for the practical guide.
Babe Addict
December 28, 2025 AT 23:00Actually, the 90% success rate for ERCP is a lie. It’s 85% in real-world settings. And ‘high-volume centers’? That’s corporate jargon. Most ERCPs are done by gastroenterologists who do 20 a year max. The FDA-approved scopes? Still get contaminated. I’ve seen the logs. The ‘disposable parts’ are just marketing. You’re still getting infected if the techs cut corners. Don’t trust the hype.
Anna Weitz
December 30, 2025 AT 22:35They say gallstones are just cholesterol crystals but they never tell you the real cause is glyphosate in your food and the toxins in your liver from processed oils. Your body makes stones because it’s trying to trap poisons. The medical system doesn’t want you to know that because then they’d have to fix the food supply not just cut out your gallbladder. Watch what you eat. Stop blaming your organs
Monika Naumann
December 31, 2025 AT 20:44It is deeply concerning that Western medicine continues to promote invasive procedures for conditions that can be managed through traditional Ayurvedic practices. In India, we have used herbal formulations like kutki and bhumiamla for centuries to dissolve gallstones naturally. The modern obsession with surgery and endoscopy reflects a systemic disregard for indigenous knowledge. One does not need a scope to heal when one has the wisdom of nature.
Kishor Raibole
January 1, 2026 AT 16:57One must contemplate the metaphysical implications of the gallbladder's removal. Is not the gallbladder the seat of courage in traditional Chinese medicine? To excise it is to sever one's inner resolve. The post-cholecystectomy syndrome is not merely physiological-it is spiritual dissonance. The bile that flows unchecked mirrors the chaos of modern life: uncontained, unfiltered, unanchored. We have forgotten that the body is a temple, not a machine to be repaired.
Satyakki Bhattacharjee
January 2, 2026 AT 23:26People get their gallbladder removed for nothing. In my village, we just eat neem leaves and turmeric milk. No surgery. No pain. No hospital bills. Why do Americans always want to cut something? The body heals itself if you stop poisoning it with cheese and fries.
Caitlin Foster
January 4, 2026 AT 01:53Wait-so you’re telling me that I don’t need to get my gallbladder out just because I had ONE episode of pain after tacos??!! And that MRCP is better than ERCP??!! And that I might still have diarrhea after surgery??!! And that 12% of people are still in pain??!! AND THAT WE’RE SPENDING $6.2 BILLION ON THIS??!! I feel like I’ve been SCAMMED!!
Robyn Hays
January 5, 2026 AT 07:53So many of us are walking around with silent stones and never know it. I found out mine were there during a routine ultrasound for something else. I was terrified-until I read this. Now I just eat more fiber, avoid fried stuff, and check in with my doc every year. No surgery. No stress. And honestly? I feel better than I did when I was ‘treatin’ my ‘digestion’ with Tums.
Jane Lucas
January 6, 2026 AT 02:21my gallbladder got removed last year and i still get the weird bloating after fatty food… i thought it was just me being weird but this post made me feel less alone. loperamide helped a bit. also i stopped eating pizza. best decision ever. also i miss pizza
Will Neitzer
January 6, 2026 AT 23:01While the clinical recommendations presented herein are largely evidence-based and commendable, one must acknowledge the limitations of the current paradigm. The reliance on imaging modalities such as MRCP and ERCP, while diagnostically robust, does not address the underlying metabolic dysregulation that precipitates cholelithiasis. A truly integrative approach-incorporating nutritional biochemistry, circadian rhythm optimization, and gut microbiome modulation-remains underexplored in mainstream gastroenterology. One wonders whether we are treating symptoms or the systemic root.
John Barron
January 7, 2026 AT 15:17EVERYTHING YOU SAID IS WRONG. 😭 The gallbladder is a detox organ. When you remove it, your liver can’t clean your blood properly. That’s why people get brain fog and depression after surgery. The FDA knows this. That’s why they approved the new scopes-so they can keep hiding the truth. I’ve had 3 ERCPs. My bile duct is scarred. They told me it was ‘normal.’ It’s not normal. It’s a cover-up. 🤫💉
Miriam Piro
January 9, 2026 AT 09:31They’re lying about the 80% silent gallstones statistic. I know a woman who had 17 stones and never felt a thing… until she died of sepsis. No warning. No pain. That’s why I say: if you’re over 40, get an ultrasound. Even if you feel fine. The system wants you to wait until you’re in ICU so they can bill you for $50k ERCPs. They profit from your ignorance. I’ve seen the spreadsheets. I’ve seen the emails. Don’t trust the doctors. Trust your gut. And get scanned.
Janice Holmes
January 11, 2026 AT 06:27Let’s be real-ERCP is the most dramatic medical procedure ever. You’re asleep. A scope goes down your throat. They cut a muscle. Pull out a stone. X-rays flash. It’s like a spy movie. And then you wake up with a sore throat and a whole new life. I had mine done last year. I’m alive. I’m free. I eat butter now. And I don’t care who knows it.
John Barron
January 12, 2026 AT 11:59Wait-so you’re saying people who get their gallbladder removed are fine? 😏 I’ve seen 3 patients who got cholecystectomies and then developed chronic fatigue, brain fog, and joint pain. The liver is overloaded. The bile is flowing where it shouldn’t. They’re calling it ‘post-cholecystectomy syndrome’ like it’s normal. It’s not normal. It’s iatrogenic. And they’re still doing 600k of these every year. Someone’s making money. And it’s not the patients.