First Aid for Tonic-Clonic Seizures: Essential Steps You Must Know

First aid for tonic-clonic seizures is a set of emergency actions designed to protect the person having the seizure, maintain a clear airway, and prevent injury until the episode ends or professional help arrives. Imagine you’re at a coffee shop and a patron suddenly starts stiffening, then jerking violently. Panic can set in fast, but knowing exactly what to do can make the difference between a brief, uneventful event and a life‑threatening situation.
Recognising a Tonic‑Clonic Seizure
Before you intervene, you need to be sure you’re dealing with a tonic‑clonic seizure, not a faint or a panic attack. A tonic‑clonic seizure typically follows this pattern:
- Loss of consciousness - the person appears unaware of their surroundings.
- Tonic phase - muscles contract, the body stiffens, and the person may let out a gasp.
- Clonic phase - rapid jerking of arms and legs lasts from 30 seconds to 2 minutes.
- Post‑ictal state - confusion, fatigue, and sometimes a headache follow the seizure.
When you see these signs, act quickly but calmly.
Immediate Safety Measures
The top priority is protecting the individual from injury. Follow these steps:
- Clear the area. Remove hard objects, sharp furniture, or anything that could cause bruises or cuts.
- Place a recovery position a safe side‑lying posture that keeps the airway open and allows fluids to drain as soon as the jerking stops. This prevents choking on saliva or vomit.
- Check the mouth. Do not insert anything - no fingers, spoons, or medication unless you’re a trained professional with a prescribed rescue drug.
- Time the seizure. If it lasts longer than five minutes, treat it as a medical emergency.
These actions buy you precious minutes while the brain’s electrical storm runs its course.
When to Call for Emergency Help
Most tonic‑clonic seizures stop on their own within two minutes, but you should dial emergency services (000 in Australia) if any of the following occur:
- The seizure lasts more than five minutes (status epilepticus a life‑threatening condition requiring immediate medical intervention).
- The person has a second seizure without regaining consciousness.
- Injury occurs - head trauma, broken bones, or severe cuts.
- Breathing stops or the person remains unresponsive after the seizure.
- It’s the first seizure the individual has ever experienced.
When you call, clearly state that the person is having a tonic‑clonic seizure and provide any known medical history, such as epilepsy or diabetes.
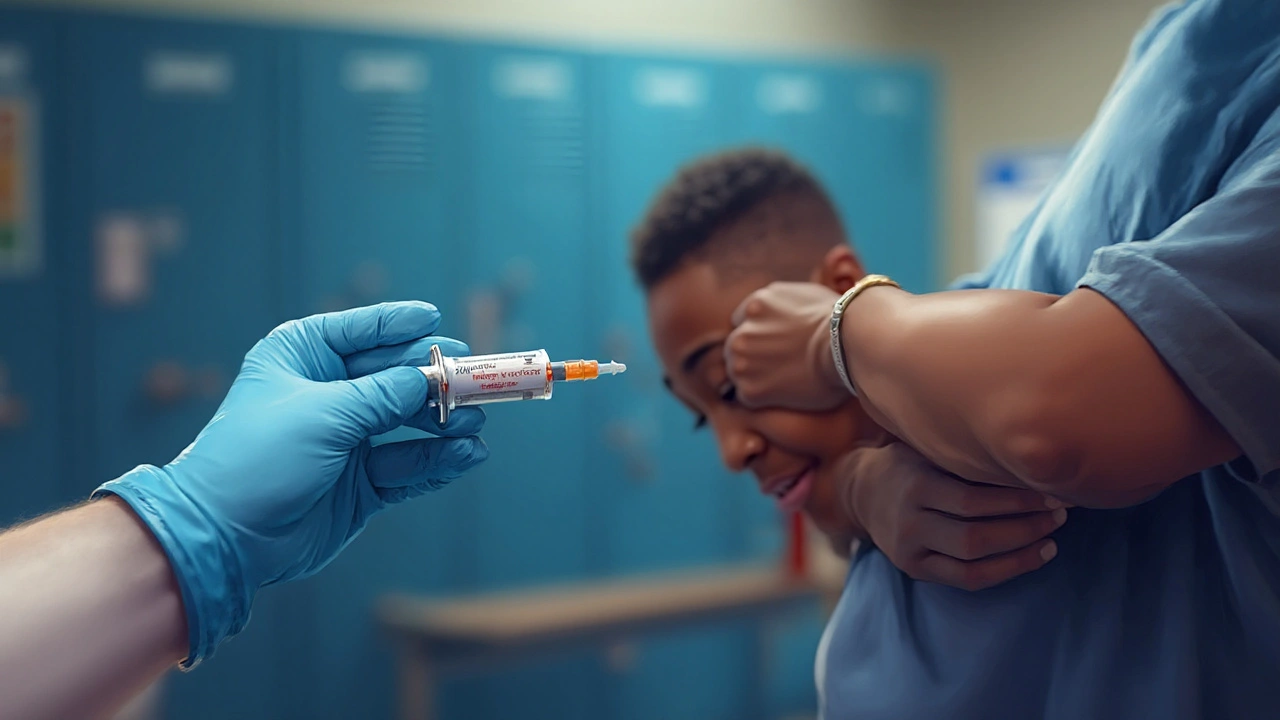
Rescue Medication: What You Need to Know
People with a known seizure disorder often carry a rescue medication, usually a benzodiazepine like midazolam a fast‑acting anti‑seizure drug administered buccally or intranasally or lorazepam. If you’re a caregiver and the medication is prescribed, you can give it when the seizure exceeds two minutes.
- Follow the dosage instructions on the prescription label.
- Administer the drug as soon as the seizure prolongs - early treatment can stop it before it becomes status epilepticus.
- Stay with the person after administration and monitor breathing.
If you’re not authorised to give medication, focus on safety and call emergency services.
Post‑Seizure Care and Monitoring
After the jerking stops, the person will enter the post‑ictal phase. Here’s how to support them:
- Keep them in the recovery position until they’re fully awake.
- Offer reassurance. Explain briefly what happened once they’re alert.
- Check blood glucose if the person is diabetic. Low blood glucose the level of sugar in the blood, measured in mg/dL can mimic or trigger seizures.
- Watch for breathing difficulties or a second seizure.
- Document the event - duration, triggers, and any injuries - for the person’s seizure diary.
Most people recover within 30 minutes, but fatigue can linger for hours.
Common Pitfalls and Myths
Even well‑meaning bystanders can unintentionally worsen the situation. Avoid these mistakes:
- Putting something in the mouth. This can cause dental injury or obstruct the airway.
- Holding the person down. The muscles contract involuntarily; restraint can cause fractures.
- Giving food or drink too soon. The gag reflex may still be suppressed.
- Assuming every loss of consciousness is a seizure. Fainting (syncope) has different causes and requires a different approach.
Remember, the goal is to protect, not to stop the convulsions directly.
Quick‑Reference Checklist for Caregivers
| Step | Action | Why It Matters |
|---|---|---|
| 1 | Protect the person from surrounding hazards | Prevents bruises, fractures, head injury |
| 2 | Time the seizure | Identifies status epilepticus (>5min) |
| 3 | Place in recovery position once jerking stops | Maintains open airway, allows fluid drainage |
| 4 | Administer rescue medication if prescribed and seizure >2min | Stops seizure early, reduces complications |
| 5 | Call emergency services if seizure >5min, injury, or repeat seizures | Ensures rapid medical intervention |
| 6 | Monitor breathing and post‑ictal recovery | Detects airway compromise or secondary seizures |
| 7 | Check blood glucose if diabetic | Rules out hypoglycaemia as a trigger |
Related Concepts and Next Steps
Understanding tonic‑clonic seizure first aid opens the door to broader seizure‑management knowledge. Topics you might explore next include:
- Epilepsy diagnosis and treatment pathways - how neurologists classify seizure types and choose long‑term medication.
- Seizure triggers and lifestyle modifications - sleep hygiene, stress reduction, and alcohol avoidance.
- Seizure‑safe environments - designing homes and schools to minimise injury risk.
- Understanding status epilepticus protocols - advanced airway management and IV benzodiazepine administration.
Each of these areas builds on the foundations you now have for emergency response.

Frequently Asked Questions
How long does a tonic‑clonic seizure usually last?
Typical seizures last between 30 seconds and two minutes. Anything beyond five minutes is considered status epilepticus and requires emergency care.
Can I give a person food or water during a seizure?
No. The gag reflex is often suppressed, so food or drink can cause choking. Wait until the person is fully alert and sitting upright.
What is the best position to place someone after a seizure?
The recovery position - lying on their side with the lower arm extended and the upper knee bent - keeps the airway clear and lets fluids drain.
When should I use rescue medication?
If a prescribed benzodiazepine is available, give it when the seizure continues past two minutes, or sooner if the person has a history of prolonged seizures.
Is it normal for the person to be confused after the seizure?
Yes. The post‑ictal state often includes confusion, fatigue, and headache. It typically resolves within 30‑60 minutes.
Can a seizure cause permanent brain damage?
A brief tonic‑clonic seizure rarely leads to permanent damage. Prolonged seizures (status epilepticus) can cause oxygen deprivation and require urgent treatment.
What should I do if the person falls and hits their head?
Call emergency services immediately. Keep the person still, monitor breathing, and avoid moving them unless they’re in immediate danger.

reshmi mahi
September 22, 2025 AT 14:12So let me get this straight-we’re supposed to just watch someone convulse like a ragdoll and *not* put anything in their mouth? What if they swallow their tongue? Oh wait-nope, that’s a myth too. Guess I’ll just stand there like a confused statue while they turn blue.
Gayle Jenkins
September 22, 2025 AT 14:55This is exactly the kind of clear, actionable guide we need. I’ve trained my whole family on this after my sister’s diagnosis. The recovery position tip? Life-changing. And PLEASE stop people from putting spoons in mouths-I saw a guy do that at a concert last year. The paramedics had to pull a plastic fork out of his throat. No. Just no.
Kaleigh Scroger
September 24, 2025 AT 14:45One thing people forget is that after the seizure ends the person is often in a deep fog and might not recognize anyone not even their own mom. Don’t crowd them. Don’t ask them 15 questions. Just sit quietly next to them and say ‘you’re safe’ once. That’s all they need. Also if they’re diabetic check their glucose but don’t shove a juice box in their face they might choke. I’ve seen it happen. It’s messy. And sad.
Cecily Bogsprocket
September 26, 2025 AT 11:55I’ve sat with people through dozens of seizures. Not as a professional but as someone who cares. What I’ve learned isn’t in any checklist-it’s that silence is the most powerful tool you have. Not the rescue meds not the positioning not even the timing. It’s the quiet presence that says ‘I’m here you’re not alone’ when the world feels like it’s collapsing. The body recovers. The mind needs more time. And sometimes all it needs is someone breathing beside it without trying to fix it.
Also if you’re gonna quote the 5-minute rule please remember that some people have baseline seizures that last 4 minutes and 40 seconds and it’s normal for them. Context matters. Not every seizure is an emergency. But if you’re unsure? Call anyway. Better safe than sorry.
And no one should ever be shamed for not knowing this. We don’t teach this in school. We should.
Edward Batchelder
September 28, 2025 AT 09:31I appreciate the clarity here, but I’m concerned about the assumption that everyone has access to rescue meds or knows someone with epilepsy. In rural areas, in low-income communities, in countries without universal healthcare-this advice can feel like a luxury. We need systemic solutions, not just individual first-aid checklists. Education, insurance access, and community training programs are what will save lives long-term.
Also, I’ve seen people get blamed for not knowing what to do-when the real failure is a society that never taught them. Let’s stop making bystanders feel guilty and start making systems more equitable.
Allison Turner
September 29, 2025 AT 05:04Wow. So much text for ‘don’t put stuff in mouths and call 911 if it lasts too long.’ I’ve seen this exact post 3 times this month. Someone’s monetizing first aid advice now?
laura lauraa
September 29, 2025 AT 07:32Oh, so now we’re supposed to be emotionally intelligent first responders while also being medically accurate? And not use emojis? What is this, a corporate compliance seminar? I’m supposed to sit calmly while someone thrashes around like a broken puppet and recite recovery position steps in my head? I’d be screaming and crying and probably hugging them-which is apparently now a violation of protocol. Also, why is everyone so obsessed with the tongue? It doesn’t swallow itself. I’ve watched enough medical dramas to know that.
Elizabeth Choi
September 30, 2025 AT 13:26According to this, 7 steps. According to the WHO, 5. According to the ILAE, 4. According to my cousin who’s a nurse, ‘just roll them and call for help.’ Why are we over-engineering this? The brain stops seizing on its own. All you need is space, time, and a phone. Everything else is performative caregiving.
Gaurav Sharma
October 1, 2025 AT 21:18It is not acceptable that the average person is expected to memorize seven steps for a medical emergency. This is a failure of public health infrastructure. I am not a nurse. I am not a paramedic. I am a citizen. Why are we burdening citizens with medical responsibilities that should be handled by trained professionals?
Edward Batchelder
October 3, 2025 AT 13:46Thank you for saying this. I’ve been saying the same thing for years. We treat emergency response like a quiz you should’ve studied for. But most people have never seen a seizure until it happens to someone they love. The real solution isn’t better checklists-it’s mandatory public health education in schools, workplaces, and community centers. We need to normalize this knowledge-not turn it into a performance of moral superiority.