Falls Risk on Anticoagulants: How to Prevent Bleeding Without Skipping Stroke Prevention
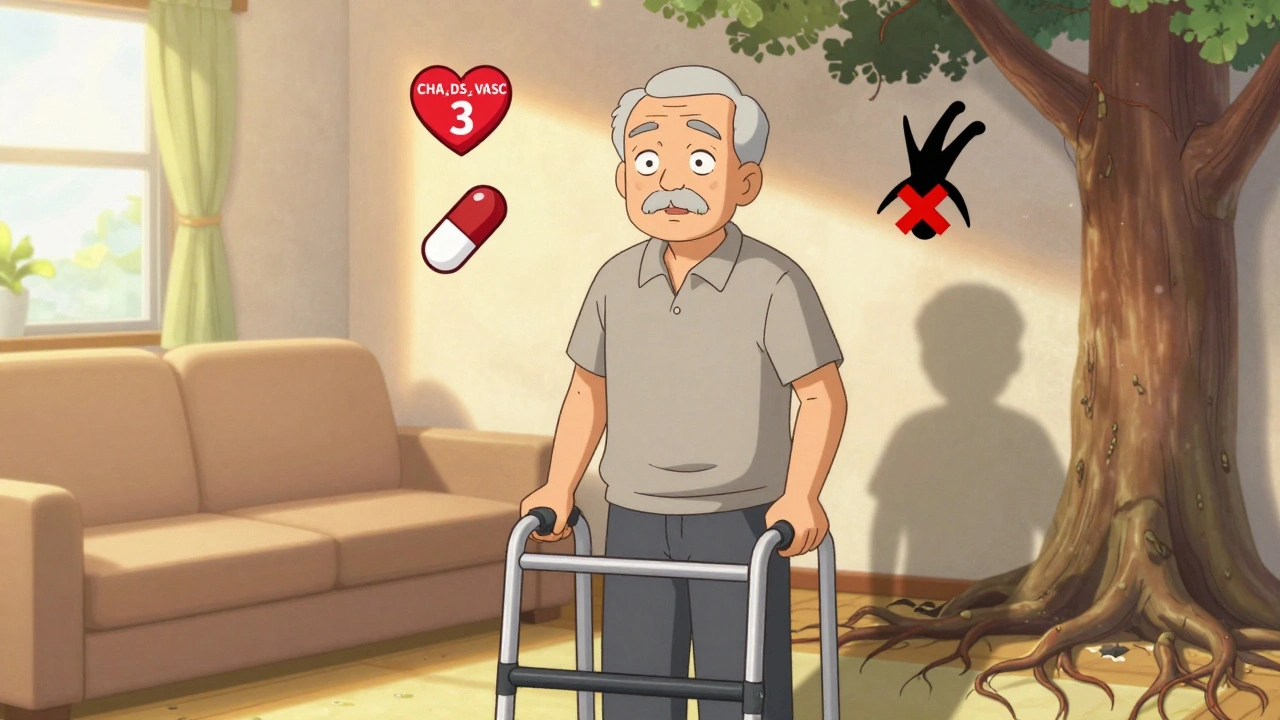
Many doctors still tell older patients with atrial fibrillation to stop their blood thinners because they’re worried about falls. But here’s the truth: fall risk alone should never be a reason to skip anticoagulation. If you’re over 65, have AFib, and your CHA₂DS₂-VASc score is 2 or higher, you’re at risk for stroke - and avoiding blood thinners because you might trip is like refusing to wear a seatbelt because you might get in a car crash. The math doesn’t add up.
Why Stopping Anticoagulants for Falls Is a Dangerous Mistake
The fear is understandable. Falls are common. About 1 in 3 adults over 65 fall each year. In nursing homes, that number jumps to more than half. And when someone on blood thinners falls, the thought of a brain bleed is terrifying. But the actual risk? It’s tiny. A 2023 review in European Geriatric Medicine found that the annual risk of intracranial hemorrhage from a fall while on anticoagulants is only 0.2% to 0.5%. Meanwhile, the risk of stroke in someone with a CHA₂DS₂-VASc score of 3 (a common score for older adults with AFib) is 3.2% per year. That’s 6 to 16 times higher. Even if you fall 295 times in one year - nearly once a day - the risk of a major bleed still doesn’t outweigh the benefit of preventing a stroke. Yet, studies show 20% to 30% of patients who clearly need anticoagulants aren’t getting them, mostly because of fall risk concerns. That’s not cautious medicine. It’s outdated fear.DOACs Are the New Standard - Especially for Fall Risks
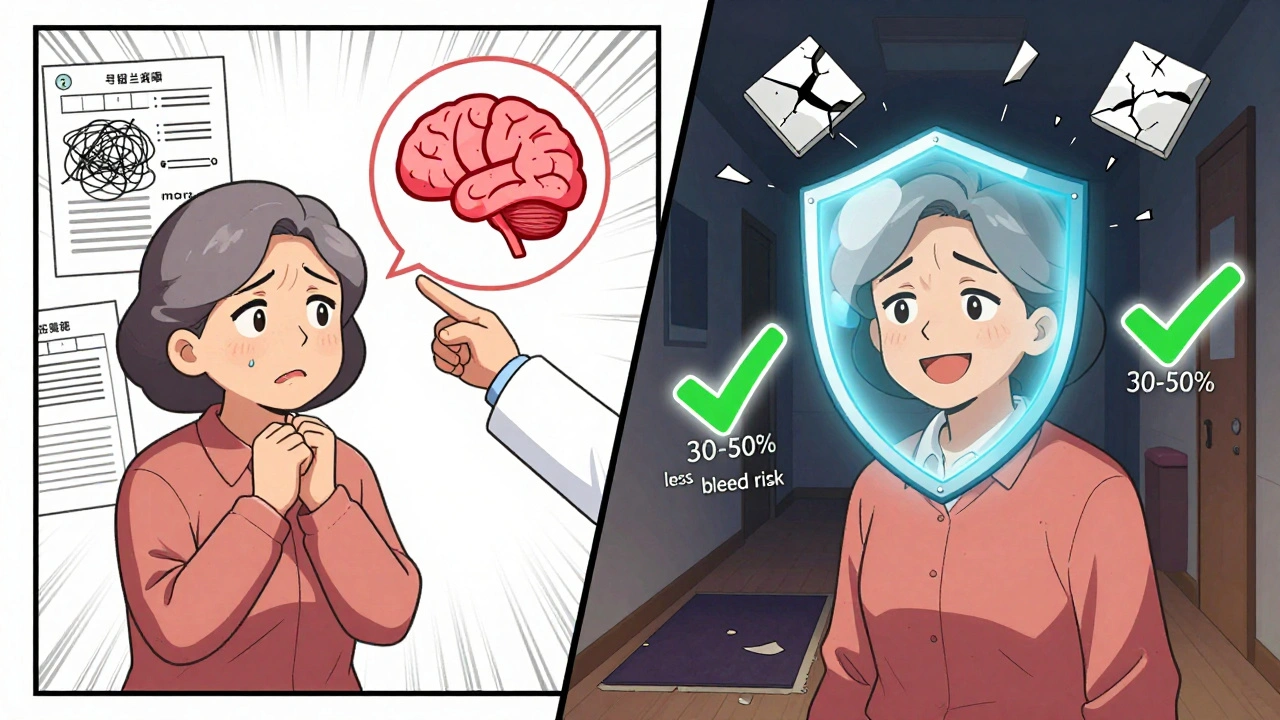
If you’re on warfarin and worried about falls, switching to a DOAC (direct oral anticoagulant) could be life-saving. These include apixaban, rivaroxaban, dabigatran, and edoxaban. They’re not just easier to take - no weekly blood tests, no dietary restrictions - they’re also safer. Compared to warfarin, DOACs reduce the risk of brain bleeding by 30% to 50%. That’s huge. In older adults who fall often, this difference isn’t just a statistical advantage - it’s the reason you can sleep better at night. In the U.S., DOACs now make up 80% of new anticoagulant prescriptions for AFib. That’s not a trend. That’s evidence. And here’s something most people don’t know: lowering the dose of a DOAC because you’re worried about bleeding doesn’t help. A 2023 review confirmed that reducing DOAC doses “has little effect on bleeding risk” but significantly lowers stroke protection. Don’t do it. Stick to the guidelines.Use the Right Tools - CHA₂DS₂-VASc and HAS-BLED
You don’t guess. You measure. Start with CHA₂DS₂-VASc. It scores your stroke risk based on:- Congestive heart failure
- Hypertension
- Age ≥75 (2 points)
- Diabetes
- Stroke or TIA history (2 points)
- Vascular disease
- Age 65-74
- Sex (female = 1 point)
- Hypertension
- Abnormal kidney or liver function
- Stroke history
- Bleeding history
- Labile INR (if on warfarin)
- Age >65
- Drugs or alcohol use
Stop Worrying About Falls - Start Preventing Them
The real solution isn’t stopping blood thinners. It’s stopping falls. A comprehensive fall risk assessment takes 30 to 60 minutes. Here’s what it should include:- Medication review - Cut out or reduce sedatives, benzodiazepines, antihypertensives, and psychotropics. These are major fall triggers.
- Gait and balance test - Use the Timed Up and Go test: time how long it takes to stand from a chair, walk 3 meters, turn, walk back, and sit down. Over 12 seconds? High fall risk.
- Vision check - Cataracts, glaucoma, or outdated glasses? Fix them.
- Home safety - Remove loose rugs, install grab bars in the bathroom, add nightlights, clear clutter from hallways.
- Orthostatic blood pressure - Check for drops when standing. If systolic pressure falls more than 20 mmHg, adjust meds or treat dehydration.
- Physical therapy - Balance training, strength exercises, tai chi - these reduce falls by up to 50%.
When Might You Skip Anticoagulation?
There are exceptions. But they’re rare. Anticoagulation should be avoided only if you have:- Active bleeding (like a stomach ulcer or recent brain bleed)
- A known bleeding disorder (like hemophilia)
- Uncontrolled high blood pressure (systolic >180 mmHg)

What Patients Really Need: Shared Decision-Making
The best outcomes happen when patients are part of the choice. A 78-year-old man with a CHA₂DS₂-VASc score of 3 was told he needed a blood thinner. He’d fallen twice in six months. He was scared. He didn’t want to die from a stroke - but he didn’t want to die from a bleed either. His doctor didn’t push. They sat down. They showed him the numbers. They talked about his home, his walker, his daily walks to the mailbox. They agreed on apixaban and scheduled a home safety visit. Six months later, he hadn’t fallen again. He was still walking his dog. That’s what good care looks like. It’s not about saying no to anticoagulation. It’s about saying yes - with eyes wide open.What Clinicians Need to Stop Doing
The Society of Hospital Medicine calls it out: “Do not routinely discontinue anticoagulation based on fall risk alone.” That’s not a suggestion. It’s a guideline. And yet, a 2023 survey found 40% to 50% of primary care providers still believe fall risk is a valid reason to withhold anticoagulants. This isn’t just ignorance. It’s systemic. Busy clinics don’t have time for full fall assessments. Nurses aren’t trained in geriatric balance testing. Electronic health records don’t prompt providers to run CHA₂DS₂-VASc scores. The fix? Start small. Add a checklist. Ask: “Has the patient’s stroke risk been scored?” “Has fall risk been addressed with a plan?” “Are we using a DOAC?” If the answer is no - pause. Don’t skip. Don’t assume. Reassess.Bottom Line: Don’t Choose Between Stroke and Falls
You don’t have to pick. You can prevent both. Anticoagulation saves lives. Falls can be managed. The two aren’t enemies - they’re problems that need two different solutions. If you’re on anticoagulants and worried about falling, talk to your doctor about:- Switching to a DOAC if you’re on warfarin
- Getting a fall risk assessment
- Reviewing your meds for fall triggers
- Starting balance exercises
- Checking your home for hazards
Should I stop my blood thinner if I fall often?
No. Falling often does not mean you should stop anticoagulation. The risk of stroke if you have atrial fibrillation and a CHA₂DS₂-VASc score of 2 or higher is far greater than the risk of a serious bleed from a fall. Instead of stopping your medication, focus on preventing falls through balance training, home safety changes, and reviewing medications that may make you unsteady.
Are DOACs safer than warfarin for people who fall?
Yes. DOACs (like apixaban and rivaroxaban) reduce the risk of brain bleeding by 30% to 50% compared to warfarin. They also don’t require regular blood tests or strict diet changes. For older adults at risk of falls, DOACs are the preferred first-line option unless kidney function is severely impaired.
Can I lower my DOAC dose to reduce bleeding risk?
No. Reducing the dose of a DOAC doesn’t significantly lower bleeding risk - but it does lower stroke protection. Guidelines strongly advise against dose reduction for fall risk alone. Always take the prescribed dose unless your doctor recommends a change based on kidney function or other medical reasons.
What’s the best way to prevent falls while on blood thinners?
Start with a multifactorial assessment: review medications that cause dizziness, test your balance with the Timed Up and Go test, check your vision, remove tripping hazards at home, and start strength and balance exercises like tai chi. Physical therapy can reduce fall risk by up to 50%.
When is it okay to not take anticoagulants despite having atrial fibrillation?
Only in rare cases: if you have active bleeding, a severe bleeding disorder, or uncontrolled high blood pressure (systolic >180 mmHg). For very frail patients with limited life expectancy (less than 1-2 years), the benefits of stroke prevention may not outweigh the burden of treatment - but this decision should be based on overall goals of care, not just fall risk.

Tommy Walton
December 2, 2025 AT 03:10Shannon Gabrielle
December 3, 2025 AT 00:11Linda Migdal
December 4, 2025 AT 11:35Louise Girvan
December 5, 2025 AT 01:06soorya Raju
December 6, 2025 AT 19:13Dennis Jesuyon Balogun
December 8, 2025 AT 00:47Grant Hurley
December 9, 2025 AT 08:47Lucinda Bresnehan
December 9, 2025 AT 17:37ANN JACOBS
December 10, 2025 AT 08:11Nnaemeka Kingsley
December 10, 2025 AT 11:59James Steele
December 12, 2025 AT 09:54