Danshen and Heart Medications: Serious Interaction Risks
Danshen Medication Interaction Checker
Check Your Medication Safety
Your Safety Assessment
Many people assume that if something is natural, it’s safe-especially when it comes to herbs. But Danshen, a traditional Chinese herb used for heart health, can be dangerously unpredictable when mixed with common heart medications. This isn’t a theoretical risk. Real patients have ended up in the ER with life-threatening bleeding after taking Danshen alongside their prescribed blood thinners.
What Exactly Is Danshen?
The active compounds-tanshinones and salvianolic acids-do have real biological effects. They can relax blood vessels, reduce inflammation, and thin the blood. That’s why people take it: to improve circulation and protect the heart. But here’s the problem: those same effects can clash violently with prescription heart drugs.
Why Danshen Is Dangerous With Blood Thinners
If you’re on warfarin (Coumadin), rivaroxaban (Xarelto), apixaban (Eliquis), or any other anticoagulant, Danshen is not an option. It doesn’t just add to the effect-it multiplies it unpredictably.
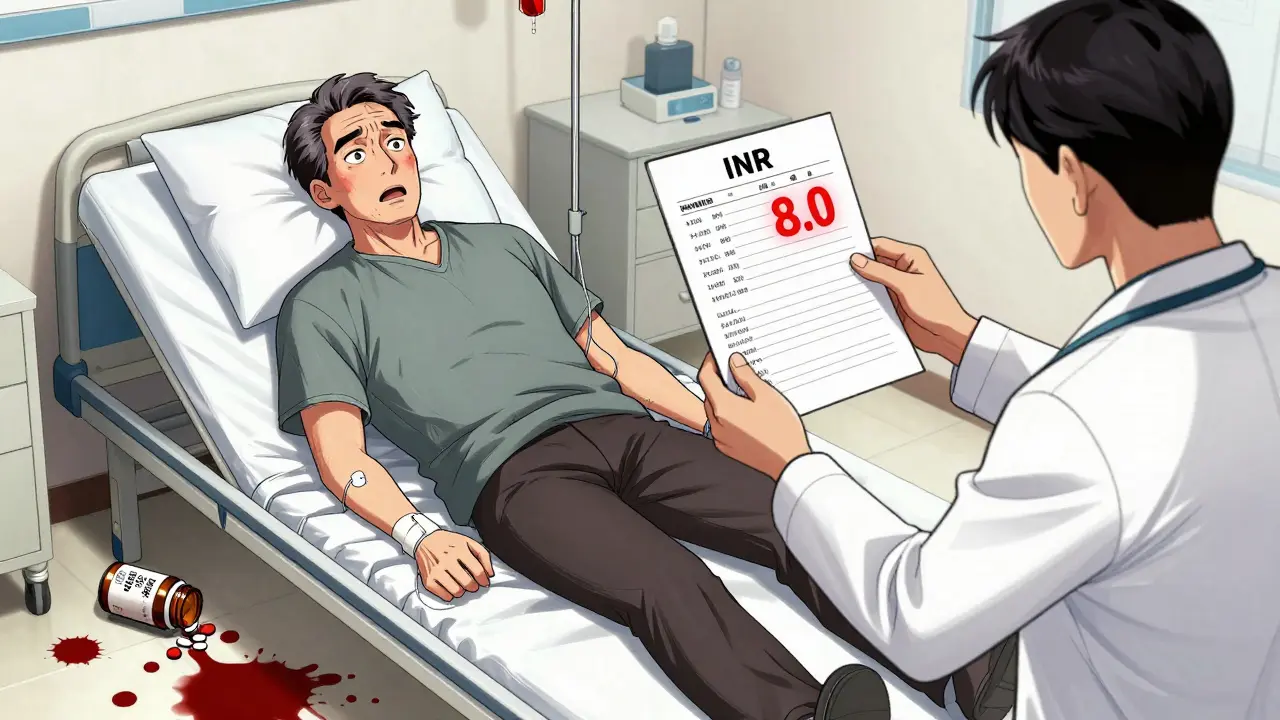
Warfarin works by blocking vitamin K, and doctors carefully adjust the dose based on regular blood tests (INR). A normal INR for someone with a mechanical heart valve is 2.5-3.5. But in documented cases, patients taking Danshen alongside warfarin saw their INR spike to over 8.0-more than double the safe upper limit. At that level, even a minor bump can cause internal bleeding.
One case involved a 62-year-old man with a mechanical mitral valve. He took Danshen for two weeks. His hemoglobin dropped from 14 to 7.6 g/dL. He needed a blood transfusion. Another patient, a 48-year-old woman, saw her INR jump from 2.8 to 5.6 after taking Danshen every other day for a month. She stopped the herb, and her INR returned to normal within days.
It’s not just warfarin. Newer drugs like rivaroxaban are also affected. Research shows Danshen blocks the liver enzyme (CYP3A4 and CYP2C9) that breaks down these medications. That means the drug stays in your system longer, building up to toxic levels. And unlike warfarin, there’s no easy way to reverse rivaroxaban’s effects if bleeding starts. No antidote. No quick fix.
Real Cases, Real Consequences
Between 2015 and 2019, researchers in Taiwan recorded 17 separate cases of dangerous Danshen-anticoagulant interactions. Patients’ INR levels rose from an average of 2.3 to 5.8-without any change in their prescription dose. One patient needed emergency surgery for a bleeding ulcer. Another had a brain bleed after a fall.
Online forums like Reddit are full of similar stories. One user wrote: “My INR went from 2.5 to 6.0 after my TCM practitioner prescribed Danshen with my Eliquis.” Another: “ER visit after taking Danshen with warfarin-never again.” These aren’t outliers. They’re predictable outcomes.

Why Patients Don’t Tell Their Doctors
Here’s the biggest hidden danger: most people don’t mention they’re taking Danshen. A 2019 study in JAMA Internal Medicine found only 28% of patients taking herbal supplements told their doctor. Why? They think it’s “just a herb.” They don’t see it as medicine. Or worse-they’re afraid their doctor will judge them.
This is especially common among Chinese immigrants. One survey found 41.7% of Chinese Americans in the U.S. regularly used Danshen while on heart meds, but only 32.4% discussed it with their physician. That’s a dangerous gap.
Doctors don’t always ask. But they should. The American College of Cardiology now recommends screening all patients on anticoagulants-especially those of Asian descent-for herbal supplement use. If you’re on blood thinners, you need to be asked directly: “Are you taking any herbs, teas, or supplements for your heart?”
Why Standardization Is Impossible
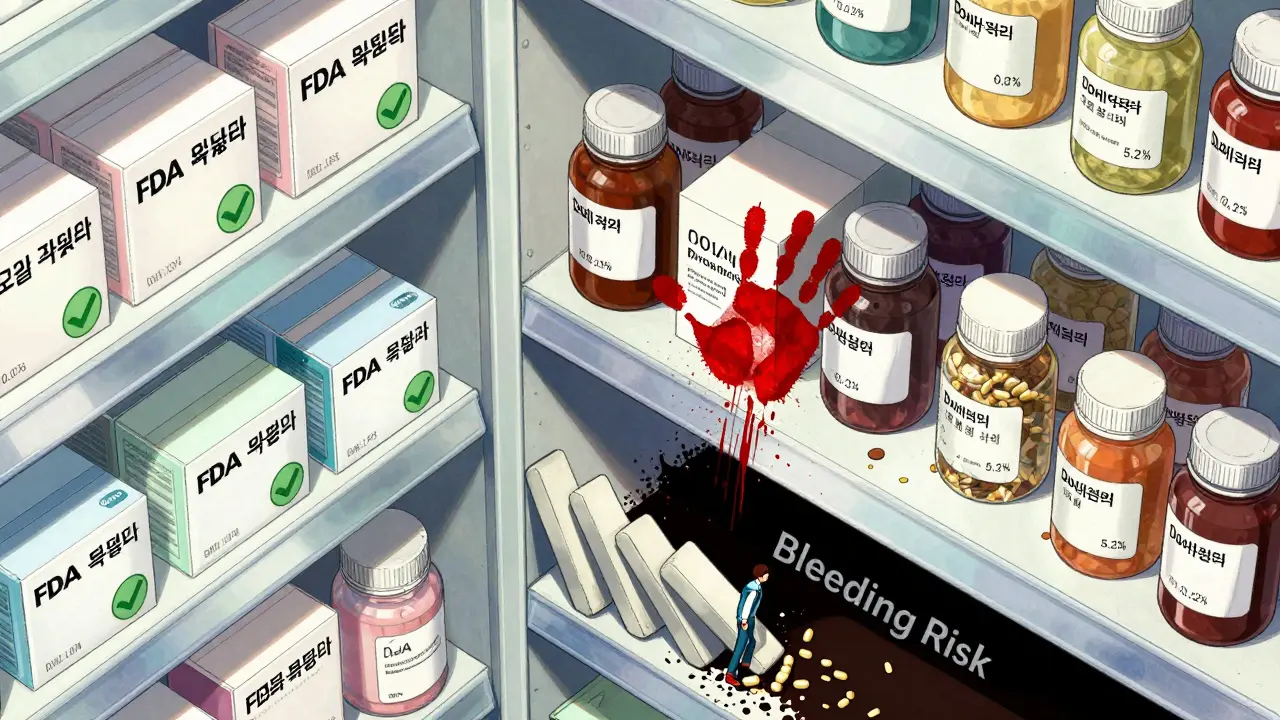
Unlike pharmaceuticals, herbal supplements aren’t held to strict quality standards. A bottle of Danshen labeled “500 mg” could contain anywhere from 0.05% to 5.2% tanshinones-the key blood-thinning compounds. That’s a 100-fold difference in potency.
One batch might be mild. The next might be strong enough to cause bleeding. There’s no way to know. No label can tell you. No dose is “safe.” The Chinese Pharmacopoeia acknowledges this variability, but U.S. manufacturers aren’t required to test or report it.
That’s why experts say there’s no established safe dose for Danshen. The RxList database says it outright: “There is not enough scientific information to determine an appropriate range of doses for danshen.”
What You Should Do
If you’re taking any blood thinner-warfarin, Xarelto, Eliquis, Pradaxa, or even aspirin-do not take Danshen. The risks are proven, serious, and avoidable.
Here’s what to do instead:
- Stop taking Danshen immediately if you’re on anticoagulants.
- Tell your doctor you’ve been using it-even if you stopped weeks ago. The effects can linger.
- Don’t replace your prescription with herbs. There’s no evidence Danshen is safer or more effective than FDA-approved medications.
- Ask for alternatives. If you want natural support for heart health, talk to your doctor about evidence-based options like omega-3s, magnesium, or CoQ10-none of which carry the same bleeding risk.
The American Heart Association says it clearly: “Natural does not mean safe.” Danshen is not an exception. It’s a warning.
What About Other Heart Medications?
Danshen doesn’t just interact with blood thinners. It can also lower blood pressure. If you’re on beta-blockers, ACE inhibitors, or calcium channel blockers, Danshen might push your blood pressure too low-leading to dizziness, fainting, or falls.
It may also interfere with statins (like atorvastatin) and antiplatelet drugs like clopidogrel. The mechanisms aren’t fully mapped yet, but the pattern is clear: Danshen messes with liver enzymes that process nearly all heart medications. That’s not coincidence. It’s chemistry.
The Bigger Picture
The global Danshen market is growing fast-projected to hit $1.84 billion by 2027. Meanwhile, more than 2.9 million Americans take warfarin alone. More than a million start new anticoagulants every year. That’s a collision waiting to happen.
China regulates Danshen as medicine. The FDA treats it as a supplement. That’s a dangerous mismatch. The European Medicines Agency requires warning labels on Danshen products about bleeding risks. The U.S. does not.
Until that changes, the burden falls on you. Don’t assume your herbalist or supplement label has your back. Your doctor doesn’t know what you’re taking unless you tell them. And if you’re on heart meds, the stakes are too high to guess.
Can I take Danshen if I’m not on blood thinners?
Even if you’re not on blood thinners, Danshen isn’t risk-free. It can lower blood pressure, affect liver enzymes, and interact with other medications like statins or diabetes drugs. If you have any chronic condition or take any prescription meds, talk to your doctor before using it. There’s no safe “just in case” use.
Is there a safer herbal alternative to Danshen for heart health?
Yes-but only under medical supervision. Omega-3 fatty acids (from fish oil) have proven benefits for heart rhythm and triglycerides. CoQ10 may help with statin-related muscle pain. Magnesium supports healthy blood pressure. None of these carry the same bleeding risk as Danshen. But they still need to be monitored if you’re on other meds.
How long does Danshen stay in my system?
There’s no definitive answer, but studies show its effects on liver enzymes can last for days after stopping. If you’re planning surgery or need to start a blood thinner, stop Danshen at least two weeks beforehand. Always tell your surgeon and anesthesiologist you used it-even if you stopped months ago.
Why do some people say Danshen helped their heart?
Some people report feeling better after taking Danshen. But that doesn’t mean it’s safe or effective. Placebo effects, natural improvement in condition, or concurrent lifestyle changes (like diet or exercise) can explain those reports. What we know for sure is that in controlled studies, Danshen increases bleeding risk when combined with heart meds. Anecdotes don’t override evidence.
What should I do if I’ve already taken Danshen with my heart medication?
Stop taking Danshen immediately. Contact your doctor or go to the ER if you notice unusual bruising, bleeding gums, nosebleeds, dark stools, or sudden weakness. Get an INR test if you’re on warfarin. Even if you feel fine, the risk of delayed bleeding is real. Don’t wait for symptoms to appear.
Final Thought
Danshen isn’t evil. It’s not a scam. It’s a powerful plant with real pharmacological effects. But that’s exactly why it’s dangerous in the wrong context. You wouldn’t mix prescription antibiotics with alcohol. You wouldn’t take insulin with a sugar binge. Don’t treat heart medications like they’re optional, and don’t treat herbs like they’re harmless. Your heart deserves better than guesswork.

Jon Paramore
December 20, 2025 AT 18:33Danshen inhibits CYP3A4 and CYP2C9 isoforms, significantly elevating plasma concentrations of direct oral anticoagulants (DOACs) like rivaroxaban. The pharmacokinetic interaction is well-documented in vitro and in case reports. INR spikes above 8.0 aren’t anomalies-they’re predictable enzyme inhibition outcomes. No dose is safe when bioavailability is unstandardized.
Swapneel Mehta
December 21, 2025 AT 10:28This is exactly why we need better public education on herbal interactions. I’ve seen elderly relatives in India take turmeric with blood thinners and think it’s harmless. The science is clear, but cultural trust in traditional remedies runs deep. We need doctors to ask, not assume.
Dan Adkins
December 21, 2025 AT 16:51It is an incontestable fact that the United States Food and Drug Administration has abdicated its responsibility to protect public health by permitting the unregulated sale of botanical agents with demonstrable pharmacological activity. The absence of mandatory potency labeling constitutes a gross dereliction of duty. This is not merely negligence-it is systemic malfeasance.
Furthermore, the normalization of self-medication with unverified phytochemicals reflects a broader cultural decay in scientific literacy. The public’s willingness to substitute anecdote for evidence is both tragic and dangerous.
Erika Putri Aldana
December 22, 2025 AT 00:24So natural = bad? Cool. Next you’ll tell me oxygen is dangerous if you breathe too much. 🤦♀️
Adrian Thompson
December 22, 2025 AT 12:18Big Pharma doesn’t want you to know herbs work better than their patented drugs. Danshen’s been used for 2000 years. Now suddenly it’s dangerous? Coincidence that the FDA approved 3 new blood thinners last year? Wake up. They’re protecting profits, not lives.
And don’t get me started on how the Chinese government regulates this stuff properly while we let corporations sell placebo crap. This is a global scam.
Teya Derksen Friesen
December 24, 2025 AT 01:54Thank you for this meticulously researched and urgently needed public service. The dissonance between traditional medicinal use and modern pharmacological understanding requires greater interdisciplinary dialogue. Healthcare providers must adopt a nonjudgmental, culturally competent approach to eliciting supplement use-particularly among immigrant populations who may perceive Western medicine as adversarial.
Standardization of herbal extracts remains an unresolved challenge. Until regulatory frameworks evolve to treat botanicals as pharmacologically active agents, the burden of safety rests unequally on the patient.
Jason Silva
December 25, 2025 AT 04:22Bro. I took Danshen for 3 months with Eliquis and felt like a superhero. No chest pain, energy like a 20-year-old. 😎 Then my doc freaked out and made me stop. Now I’m back to feeling like a zombie. Who’s really being reckless here? 🤔
Cameron Hoover
December 25, 2025 AT 20:39I used to think herbs were just ‘natural medicine’ until my uncle had a brain bleed after mixing Danshen with warfarin. He didn’t tell anyone. Didn’t even know it could do that. Now I’m the guy who asks everyone: ‘What else are you taking?’ Because silence kills. This isn’t fear-mongering-it’s harm reduction.
Stacey Smith
December 26, 2025 AT 23:23Stop the herbal nonsense. If you want heart health, exercise, eat real food, and take your damn pills. No magic roots are worth your life.
Ben Warren
December 27, 2025 AT 17:06It is regrettable that the prevailing cultural narrative surrounding herbal supplementation has co-opted the language of wellness to obscure the fundamental principles of pharmacology. The assertion that ‘natural’ equates to ‘safe’ is not only scientifically indefensible but epistemologically hazardous. The absence of regulatory oversight in the dietary supplement industry has created a permissive environment wherein the bioactive constituents of botanicals-many of which exhibit potent, dose-dependent, and pharmacodynamically complex effects-are consumed with the same casualness as a multivitamin. This is not merely a failure of education; it is a systemic failure of risk communication.
Furthermore, the anecdotal reports of subjective improvement following Danshen ingestion must be contextualized within the framework of cognitive biases: confirmation bias, regression to the mean, and the placebo effect. The documented clinical outcomes-hemorrhagic events, INR escalation, and multi-organ failure-are not subject to interpretation. They are data. They are outcomes. They are non-negotiable.
It is incumbent upon the medical community to move beyond passive inquiry and implement mandatory, structured screening protocols for all patients on anticoagulant therapy. The burden of disclosure must not rest upon the patient’s willingness to disclose what they perceive as ‘non-medical’ interventions. The onus is on the clinician to ask, to document, and to educate. Anything less is malpractice.