Corticosteroids for Autoimmune Disease: Benefits and Long-Term Effects

When your immune system turns against your own body, things get messy fast. Autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis don’t just cause pain-they can shut down organs, wreck joints, and steal your energy. That’s where corticosteroids come in. These aren’t the muscle-building steroids athletes misuse. These are powerful anti-inflammatory drugs that mimic your body’s natural stress hormone, cortisol. They’re fast, they’re strong, and for many people, they’re the difference between being bedridden and being able to pick up their kid from school.
How Corticosteroids Actually Work
Corticosteroids like prednisone and methylprednisolone don’t just mask symptoms. They hit the brakes on your immune system at the molecular level. Inside your cells, they bind to receptors that control gene activity. This shuts down the production of inflammatory proteins-things like tumor necrosis factor and interleukins-that cause swelling, redness, and tissue damage. They also block enzymes like phospholipase A2, which is behind the chain reaction that turns minor irritation into full-blown inflammation.
Unlike drugs like methotrexate or azathioprine, which can take weeks to kick in, corticosteroids work in hours. A patient with sudden kidney inflammation from lupus might wake up with swollen ankles and feel like they’re drowning in fluid. After one dose of IV methylprednisolone, the swelling drops by half in 24 hours. That’s not magic-it’s science. This speed is why doctors reach for corticosteroids first when someone shows up in the ER with a flare-up.
When They Work Best
Corticosteroids shine in acute, severe autoimmune flares. For conditions like Wegener’s granulomatosis, Goodpasture’s syndrome, or rapidly progressive glomerulonephritis, high-dose pulses of methylprednisolone are often the first line of defense. They’re combined with drugs like cyclophosphamide to kill off the rogue immune cells causing the damage. In rheumatoid arthritis, they’re used short-term to control joint pain while slower-acting drugs take effect.
They’re also critical in asthma attacks, severe allergic reactions, and skin conditions like pemphigus. Even in diseases like multiple sclerosis, where nerve damage is permanent, corticosteroids can shorten the length of a relapse and speed up recovery. But here’s the catch: they don’t fix the root problem. They just quiet the noise.
Where They Don’t Help
Not every autoimmune disease responds. Corticosteroids won’t reverse advanced type 1 diabetes where the pancreas is already destroyed. They won’t bring back thyroid function in late-stage Hashimoto’s. In advanced primary biliary cholangitis, where bile ducts are scarred beyond repair, steroids offer little more than temporary relief. The same goes for Graves’ disease-thyroid overactivity won’t calm down with steroids alone.
This isn’t a failure of the drug. It’s a limitation of the disease. If the damage is done and the cells are gone, no amount of inflammation control will bring them back. That’s why early diagnosis matters. Corticosteroids are most effective when used before irreversible harm sets in.
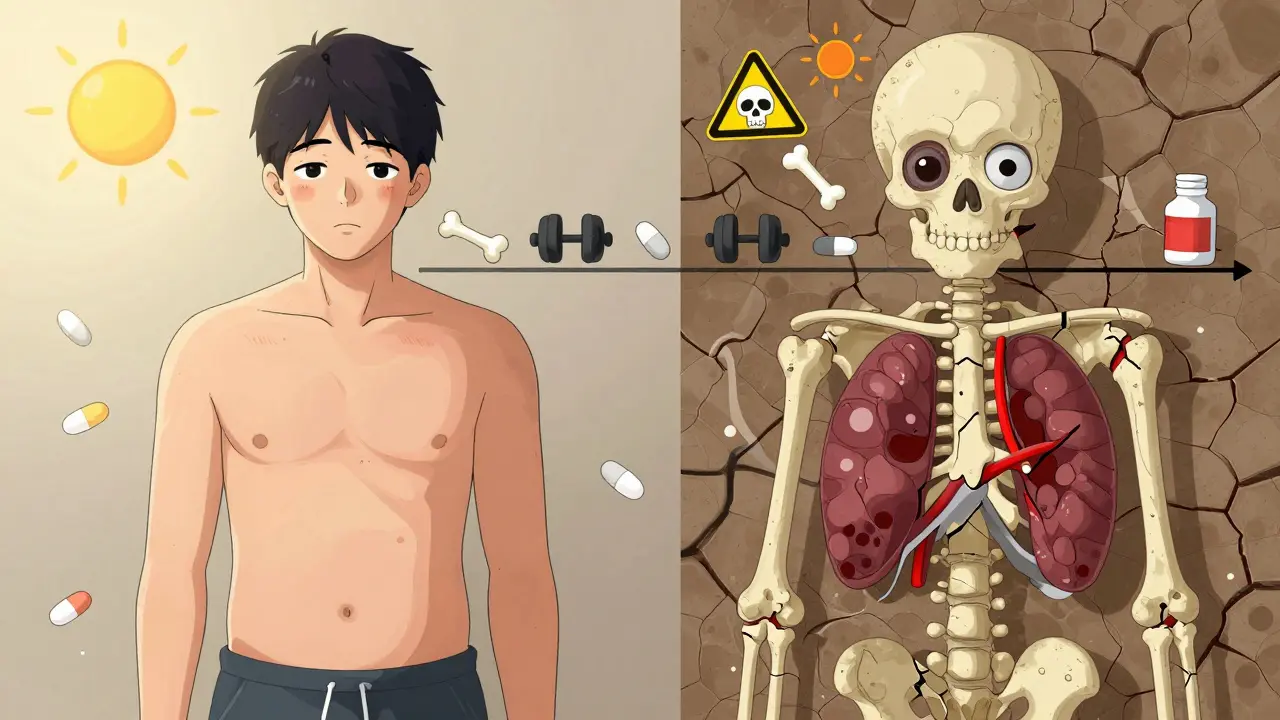
The Hidden Cost: Long-Term Side Effects
Here’s the truth no one tells you until you’ve been on them for months: corticosteroids wear you down. The longer you take them, the more your body pays.
Bones weaken. Osteoporosis isn’t just a risk-it’s almost guaranteed if you’re on more than 5 mg of prednisone daily for over six months. One study found that 30-50% of long-term users break a bone. That’s why doctors now push calcium, vitamin D, and bisphosphonates from day one.
Your eyes change. Cataracts develop faster. Glaucoma risk goes up. You might not notice it until your vision gets blurry, and by then, it’s permanent.
Your metabolism goes haywire. Weight gain isn’t just from eating more-it’s fluid retention and fat redistribution. That moon face, buffalo hump, and belly fat? That’s not laziness. That’s the drug. Blood sugar spikes. Diabetics struggle. Prediabetics may get pushed over the edge.
Your adrenal glands forget how to work. Your body stops making its own cortisol because the drug is doing it for you. If you stop suddenly, you can crash-low blood pressure, nausea, even death. That’s why tapering isn’t optional. It’s life-saving.
And then there’s the skin. Thinning. Easy bruising. Slow healing. Sun sensitivity. One patient in Perth told me she stopped going to the beach because her skin blistered after 15 minutes. That’s not an exaggeration-it’s common.
How Doctors Try to Reduce the Damage
No one wants to be on corticosteroids forever. That’s why modern treatment isn’t about steroids alone-it’s about steroids as a bridge.
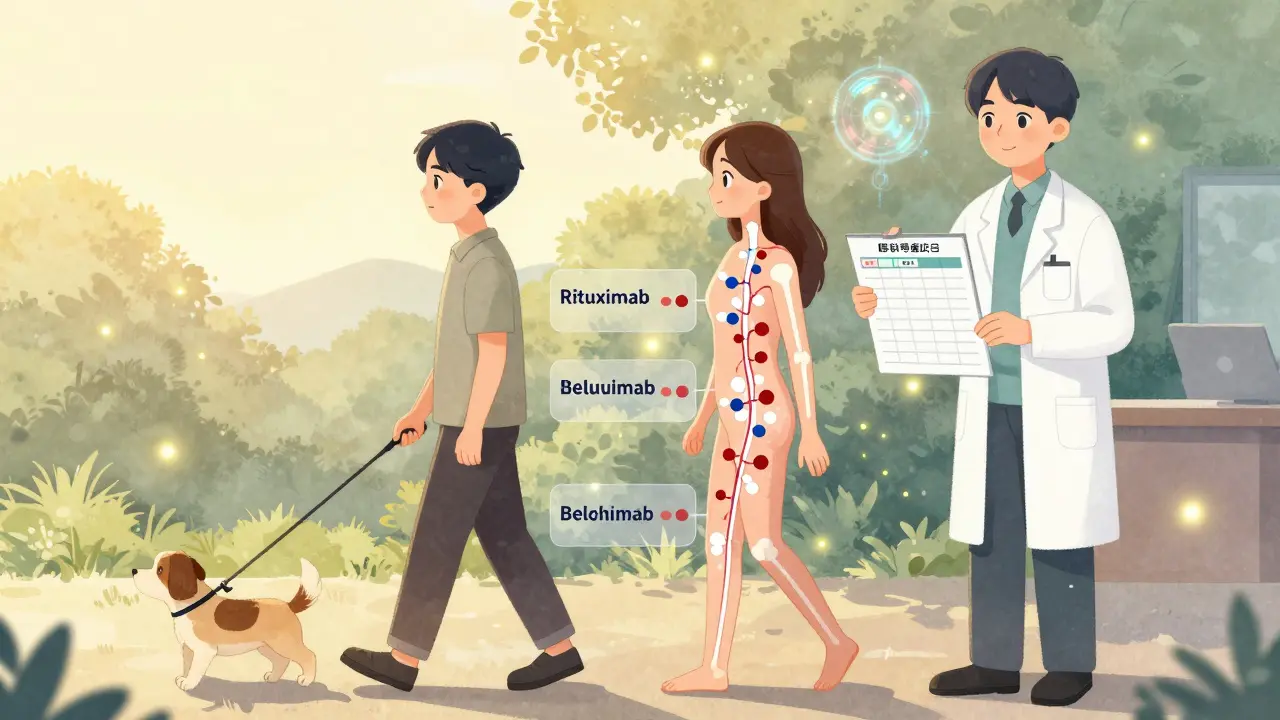
Doctors now pair them with drugs like methotrexate, azathioprine, or rituximab. These drugs take longer to work but let you drop the steroid dose faster. In autoimmune hemolytic anemia, adding rituximab to prednisone doubled the time patients stayed in remission.
Topical versions help too. Inhaled steroids for asthma, creams for eczema, eye drops for uveitis-these deliver the medicine where it’s needed and minimize what hits your bloodstream. Less systemic exposure means fewer side effects.
And there’s new research on GILZ, a protein triggered by corticosteroids that controls inflammation. Scientists are working on synthetic versions that might give the anti-inflammatory effect without the bone loss or weight gain. It’s early, but it’s promising.
What You Can Do to Protect Yourself
If you’re on corticosteroids, you’re not powerless. Here’s what actually helps:
- Take the lowest dose possible. Your doctor should be aiming for the minimum effective dose, not the highest that works.
- Never stop cold turkey. Tapering takes weeks or months. Ask for a written plan.
- Get a bone density scan every year. Start calcium and vitamin D supplements early.
- Exercise. Weight-bearing activity like walking or resistance training helps keep bones strong.
- Watch your sugar and salt intake. Steroids make you retain fluid and raise blood sugar.
- Use sunscreen daily. Even on cloudy days. Your skin is more vulnerable.
- Carry a medical alert card. In an emergency, doctors need to know you’re on steroids.
One patient I spoke with in Fremantle cut her prednisone dose from 20 mg to 5 mg over eight months. She didn’t feel perfect-but she didn’t collapse either. She walked her dog every morning. She slept through the night. She kept her job. That’s the goal: not a cure, but a life.
The Future: Less Steroids, More Precision
The field is shifting. New biologics like rituximab, belimumab, and anifrolumab are replacing steroids in some diseases. They’re targeted. They’re expensive. But they don’t wreck your bones.
For now, corticosteroids remain the most powerful tool we have to stop an autoimmune flare in its tracks. But they’re not a long-term solution. They’re a fire extinguisher-not a home renovation.
The smartest doctors don’t just prescribe steroids. They plan their exit. They set targets: reduce proteinuria by 50%, improve lung function by 20%, lower joint swelling to a 2 on a 10-point scale. Once those targets are hit, they start cutting the dose-slowly, carefully, with monitoring.
It’s not about fear. It’s about balance. You need to control the disease without destroying your body in the process.
Are corticosteroids the same as anabolic steroids?
No. Anabolic steroids mimic testosterone and are used to build muscle. Corticosteroids mimic cortisol and are used to reduce inflammation and suppress the immune system. They have completely different effects and uses.
How long can you safely take corticosteroids?
Short-term use-under three weeks-is generally safe. For longer use, doctors aim to keep doses below 5 mg of prednisone per day and combine them with other drugs to reduce dependency. The goal is always to taper off completely, but some patients need low doses indefinitely. The key is minimizing the dose and monitoring for side effects.
Can corticosteroids cause weight gain even if I eat normally?
Yes. Corticosteroids change how your body stores fat and retains fluid. You may gain weight around your face, neck, and belly even if your diet doesn’t change. This is a direct effect of the drug, not overeating.
Why do I need to taper off corticosteroids instead of stopping suddenly?
Your adrenal glands stop making cortisol when you’re on long-term steroids. Stopping suddenly leaves your body without enough of this vital hormone, which can cause adrenal crisis-low blood pressure, vomiting, confusion, and even death. Tapering lets your glands slowly wake up again.
Do corticosteroids work for all autoimmune diseases?
No. They’re ineffective in advanced stages of type 1 diabetes, Hashimoto’s thyroiditis, Graves’ disease, and advanced primary biliary cholangitis. They work best when inflammation is the main problem and the target organs still have some function left.
Is there a way to avoid the side effects of corticosteroids?
You can’t avoid them entirely, but you can reduce them. Use the lowest effective dose, combine with other drugs, use topical versions when possible, take calcium and vitamin D, exercise, avoid smoking, and get regular bone and eye checks. Newer targeted therapies are also reducing the need for high-dose steroids.
If you’re on corticosteroids, you’re not alone. Thousands of people manage them every day-some for months, others for years. The goal isn’t perfection. It’s control. Control of the disease. Control of the side effects. And most of all, control over your life.

Demetria Morris
February 4, 2026 AT 01:42People don’t realize how dangerous these drugs are until it’s too late. I watched my aunt go from hiking every weekend to needing a cane because her hips shattered from osteoporosis. They called it ‘side effects’ like it was a minor inconvenience. It’s not. It’s a slow-motion destruction of your body, and doctors act like it’s just part of the deal.