Chronic Alcohol Use Disorder: Health Risks and Treatment Options
Chronic Alcohol Use Disorder isn’t just about drinking too much. It’s a medical condition where your brain and body become wired to need alcohol-even when it’s destroying your health, relationships, and life. This isn’t a lack of willpower. It’s a brain disease. And like diabetes or heart disease, it needs treatment-not judgment.
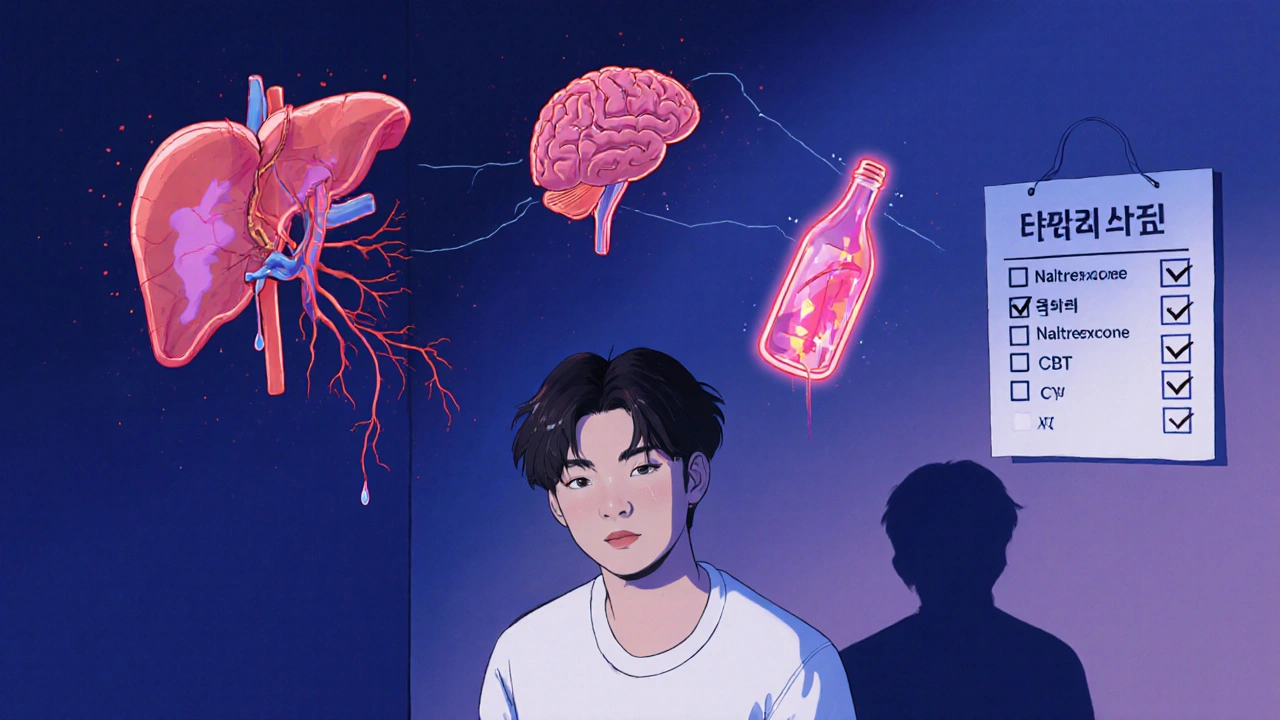
How Alcohol Changes Your Brain
When you drink regularly, your brain adapts. At first, alcohol feels relaxing. But over time, your brain starts producing less of its own natural calming chemicals because alcohol is doing it for you. That’s when tolerance kicks in: you need more to feel the same effect. Then comes dependence. Your brain now expects alcohol to be there. Stop drinking, and your nervous system goes into overdrive. That’s withdrawal.
Withdrawal isn’t just feeling shaky. It can mean seizures, hallucinations, or delirium tremens-a life-threatening state of confusion, rapid heartbeat, and high fever. The risk is highest 48 to 72 hours after your last drink. That’s why quitting cold turkey can be deadly. Medically supervised detox is often the first step.
The Body Breakdown: Organs Under Attack
Alcohol doesn’t just affect your head. It attacks your whole body.
Your liver takes the biggest hit. After years of heavy drinking, nearly everyone develops fatty liver. That’s reversible-if you stop. But for many, it moves to alcoholic hepatitis: inflamed, swollen liver cells. Then comes cirrhosis. Scar tissue replaces healthy liver tissue. The liver can’t filter toxins, make proteins, or store energy. Once cirrhosis sets in, damage is often permanent. Even if you quit, your liver may never fully recover.
Your heart isn’t safe either. Heavy drinking raises blood pressure, causes irregular heart rhythms like atrial fibrillation, and weakens heart muscle. That increases stroke risk by 34% and heart attack risk significantly. Even moderate drinking over time can do damage.
Then there’s the brain. Long-term alcohol use shrinks brain tissue. Memory fades. Thinking slows. Some people develop Wernicke-Korsakoff syndrome-a severe brain disorder caused by thiamine (vitamin B1) deficiency. Symptoms include confusion, loss of coordination, and eye problems. It’s preventable with proper nutrition and stopping alcohol.
Your pancreas, immune system, and digestive tract all suffer too. Alcohol increases your risk of pancreatitis, pneumonia, and cancers of the mouth, throat, liver, breast, and bowel. Heavy drinkers are five times more likely to get mouth cancer. Each daily drink raises breast cancer risk by 12%.
Mental Health and the Hidden Toll
Alcohol doesn’t just numb your body-it numbs your life. Many people with Chronic Alcohol Use Disorder also struggle with depression, anxiety, or trauma. Alcohol might seem like a way to cope, but it makes these conditions worse over time.
Relationships fall apart. Jobs are lost. Finances collapse. Homelessness becomes a real risk. Studies show people with AUD are 2.7 times more likely to get pneumonia because their immune system is weakened. They’re also more likely to be victims of violence or to cause it.
And then there’s the stigma. Many think AUD is a moral failure. It’s not. It’s a brain disorder shaped by biology, environment, and genetics. People don’t choose to lose control. They lose it because their brain has been rewired.
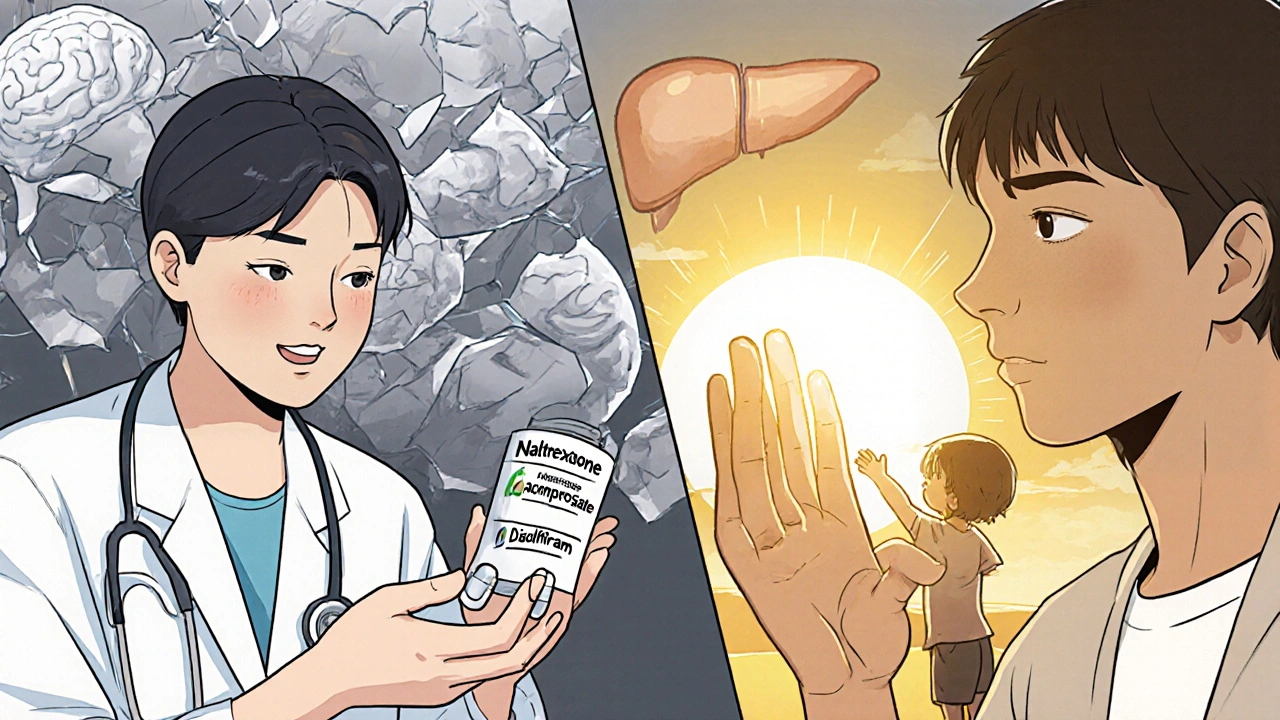
Treatment That Works: It’s Not One-Size-Fits-All
Recovery isn’t about hitting rock bottom. It’s about finding the right help at the right time. Treatment works-and it’s more effective than most people realize.
Three FDA-approved medications are proven to help:
- Naltrexone blocks the pleasurable effects of alcohol, reducing cravings.
- Acamprosate helps stabilize brain chemistry after quitting.
- Disulfiram makes drinking unpleasant-it causes nausea, flushing, and headaches if alcohol is consumed.
These aren’t magic pills. They work best with therapy.
Cognitive Behavioral Therapy (CBT) helps people recognize triggers and change how they respond. Studies show CBT reduces heavy drinking days by 60%. Motivational Enhancement Therapy helps people find their own reasons to quit-because real change comes from within.
Support groups like Alcoholics Anonymous (AA) have helped millions since 1935. While exact success rates are debated, many find long-term recovery through the structure, community, and accountability AA provides. Newer digital tools like the reSET app have shown 40.7% abstinence rates in clinical trials-nearly double the rate of standard care.
Emerging Treatments: What’s Next?
Treatment is evolving. Transcranial Magnetic Stimulation (TMS), a non-invasive brain stimulation technique, showed 50% abstinence rates in a 2022 study. It targets brain areas involved in cravings. It’s not widely available yet, but it’s a promising step.
Another breakthrough? Combining medication with therapy. The MATTERS study found this combo increased abstinence rates by 24% compared to either treatment alone. That’s huge. It means treatment isn’t about picking one thing-it’s about layering support.
And recovery doesn’t mean perfection. Relapse is common. It doesn’t mean failure. It means the treatment plan needs adjusting. Think of it like managing high blood pressure-you don’t stop taking medicine after one good week.

Reversing Damage: Is It Too Late?
Many people think if they’ve had cirrhosis or nerve damage, it’s too late. That’s not true.
The liver is one of the few organs that can regenerate. If you stop drinking early enough-even with early cirrhosis-your liver can heal significantly. Some people see improvements in liver function within months.
Nerve damage from alcohol can also improve. Tingling, numbness, or pain in hands and feet? It may fade over time with sobriety and proper nutrition. Thiamine supplements can reverse early brain damage from Wernicke’s encephalopathy.
But the clock is ticking. The longer you wait, the harder recovery becomes. The damage becomes permanent. That’s why early intervention saves lives.
Getting Help: Where to Start
If you or someone you care about is struggling, here’s how to begin:
- See a doctor. Don’t try to quit alone if you’ve been drinking heavily for months or years. Withdrawal can be deadly.
- Ask about medications. Naltrexone, acamprosate, and disulfiram are safe and effective. Many primary care doctors can prescribe them.
- Find a therapist. Look for someone trained in CBT or MET for AUD.
- Explore support groups. AA, SMART Recovery, and online communities offer free, ongoing support.
- Check for local programs. Many hospitals and clinics offer outpatient AUD treatment. No insurance? Some programs are sliding-scale or free.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) offers free resources at RethinkingDrinking.nih.gov. It’s not about labeling yourself an alcoholic. It’s about understanding your drinking and making informed choices.
You’re Not Alone
Over 14 million Americans have Chronic Alcohol Use Disorder. Only 19% get treatment. That’s not because they don’t want help. It’s because help is hard to find, or they’re afraid to ask.
Recovery isn’t about becoming perfect. It’s about choosing life over addiction. One day at a time. One healthy meal. One sleepless night survived. One call to a counselor.
The body can heal. The mind can rewire. The future doesn’t have to look like the past.
Can you recover from alcohol use disorder without professional help?
Some people do quit on their own, especially with mild AUD. But for moderate to severe cases, professional help dramatically increases success. Withdrawal can be dangerous, and cravings are powerful. Medications and therapy reduce relapse risk by up to 50%. Trying alone isn’t a sign of strength-it’s a risk.
How long does it take to recover from alcohol use disorder?
Recovery isn’t measured in weeks or months. It’s a lifelong process. Physical withdrawal lasts days to weeks. Brain chemistry takes months to stabilize. Cravings can return years later. But many people reach a point where alcohol no longer controls their life. That’s recovery. It’s not about never drinking again-it’s about never letting it take over again.
Is it safe to quit drinking cold turkey?
If you’ve been drinking heavily for months or years, quitting cold turkey can be life-threatening. Seizures, delirium tremens, and heart rhythm problems can occur. Always seek medical advice before stopping. A doctor can guide you through safe detox, often with medications to ease symptoms.
Do alcohol medications just replace one addiction with another?
No. Medications like naltrexone and acamprosate don’t create a high or dependence. They help reduce cravings and stabilize brain chemistry. Think of them like insulin for diabetes-they treat the condition, not replace it. They’re used short-term or long-term based on need, under medical supervision.
Can alcohol damage be reversed?
Yes-some of it. Fatty liver can reverse within weeks of quitting. Early inflammation (hepatitis) can improve. Nerve damage and brain function can partially recover. But advanced cirrhosis and permanent brain damage may not fully heal. The earlier you stop, the better your chances. Quitting at any stage is better than continuing.
What’s the difference between alcohol abuse and alcohol use disorder?
The term "alcohol abuse" was removed from medical guidelines in 2013. Now, it’s all called Alcohol Use Disorder (AUD), with mild, moderate, or severe levels based on how many symptoms you have. It’s not about how much you drink-it’s about how alcohol affects your life. Losing control, ignoring consequences, or needing alcohol to feel normal? That’s AUD, no matter the quantity.
Are there alternatives to Alcoholics Anonymous?
Yes. SMART Recovery uses science-based tools to build self-reliance. LifeRing focuses on sobriety without spirituality. Women for Sobriety offers gender-specific support. Online groups and apps like reSET provide flexible, anonymous help. You don’t have to fit into one model-find what works for you.

Conor McNamara
November 18, 2025 AT 00:54they say it's a brain disease but i think the pharma giants just want you hooked on meds so they can sell naltrexone for 500 bucks a month... i saw a doc on youtube who said the liver heals faster if you drink coconut water and do cold showers... they don't want you to know that.
steffi walsh
November 18, 2025 AT 01:19you’re not alone 💪 i was in the same spot 3 years ago-shaky hands, lost my job, thought i was doomed. started with a doctor, got on naltrexone, went to SMART Recovery meetings online. now i hike every weekend. it’s not perfect, but i’m alive. one day at a time 😊
Leilani O'Neill
November 19, 2025 AT 13:07How quaint. In my country, people who can’t control their drinking are just weak. No amount of therapy or fancy meds fixes moral failure. You don’t get to call it a 'disease' and then expect sympathy while you drain public healthcare. Quit or get out.
Riohlo (Or Rio) Marie
November 21, 2025 AT 10:26Oh darling, let me dissect this for you. The entire framework here is bourgeois neoliberal nonsense-reducing a profound existential collapse into a pharmacological checklist. Naltrexone? Please. It’s just chemical repression. True liberation comes from shadow work, ancestral trauma release, and a 14-day juice cleanse in Sedona. Also, the NIH? Totally funded by Big Pharma. You’re being manipulated by the system, sweetie.
Kristi Joy
November 21, 2025 AT 20:49steffi walsh, your comment made me cry a little. you’re so right-recovery isn’t about perfection. i’ve been sober 18 months and still have days where the craving hits like a truck. but i call my sponsor, go for a walk, and remind myself: i’m not broken. i’m healing. thank you for saying that.
Hal Nicholas
November 22, 2025 AT 15:31conor mcnamara, you’re an idiot. the 'coconut water cure' is a scam. i’ve seen 12 people die from DTs because they listened to YouTube gurus instead of doctors. stop spreading dangerous nonsense. this isn’t a tiktok trend-it’s life or death.
Kristina Williams
November 24, 2025 AT 03:03they’re all lying. the government made alcohol a disease so they could control us. if you quit, they lose their tax money. also, i heard the liver doesn’t regenerate-it’s a lie. they just want you to think you’re fixed so you stop asking questions.
Louie Amour
November 25, 2025 AT 19:15you people are pathetic. you think therapy and apps fix anything? i’ve been clean for 7 years. i didn’t need meds. i didn’t need AA. i just looked in the mirror one day and said, 'enough.' you’re all just looking for excuses. stop blaming the brain. take responsibility.