Biologic Infusion Reactions: How to Prevent and Handle Emergency Responses

Biologic Infusion Reaction Risk Calculator
How likely is a reaction?
This tool estimates your risk of a biologic infusion reaction based on your treatment history and medical details. Results are for informational purposes only and should not replace professional medical advice.
Your Estimated Reaction Risk
Tips to reduce risk:
- Request steroid premedication (hydrocortisone/methylprednisolone)
- Ask for slow infusion rates (10-15 mL/min)
- Ensure you're hydrated with normal saline
- Discuss desensitization if you've had a reaction
When you’re on a biologic for rheumatoid arthritis, Crohn’s disease, or cancer, it’s supposed to help you feel better. But for up to 4 in 10 people, the very treatment that’s saving their life can trigger a scary reaction during the infusion. Flushing, chills, chest tightness, low blood pressure-these aren’t just side effects. They’re warning signs that demand quick action. The good news? With the right steps, most of these reactions can be stopped before they turn dangerous-and you can keep getting the treatment you need.
What Exactly Is a Biologic Infusion Reaction?
Biologic infusion reactions happen when your immune system reacts to drugs made from living cells-like monoclonal antibodies (infliximab, rituximab, trastuzumab) or fusion proteins (etanercept). These aren’t regular pills. They’re given slowly through an IV, and your body sometimes sees them as invaders. There are three main types:- Immediate hypersensitivity reactions (within 1-2 hours): Think hives, itching, swelling, trouble breathing. Often caused by IgE antibodies or other immune triggers.
- Cytokine release syndrome (minutes to hours): Fever, chills, low blood pressure, muscle aches. Happens when your immune cells go into overdrive and dump out inflammatory signals.
- Delayed reactions (24-72 hours later): Rash, joint pain, fatigue. Less urgent but still need attention.
Who’s at Risk?
Not everyone gets these reactions. But some factors raise your odds:- First infusion: Your body hasn’t seen the drug yet. Rituximab has a 30-80% reaction rate on the first go.
- Drug type: TNF inhibitors like infliximab cause reactions in 10-20% of patients. Cetuximab? Up to 25%, with 1-5% severe cases in people with pre-existing IgE antibodies.
- Previous reactions: If you had one before, you’re more likely to have another.
- Infusion speed: Too fast = higher risk. Slower starts cut reaction rates by half.
How to Prevent Reactions Before They Start
Prevention isn’t guesswork. It’s science-backed and standardized. The gold-standard premedication combo includes:- Hydrocortisone 200 mg IV or methylprednisolone 125 mg IV given 30 minutes before the infusion. This reduces antibody development by 47% compared to no steroid.
- Diphenhydramine 50 mg IV or cetirizine 10 mg oral given 1 hour before. Cetirizine works just as well as diphenhydramine but causes 78% less drowsiness.
- Acetaminophen 1,000 mg oral 1 hour before to reduce fever and chills.

What to Do If a Reaction Happens
If you feel anything unusual during your infusion-flushing, tight chest, dizziness, nausea-tell the nurse immediately. Don’t wait. Don’t think it’s "just a little uncomfortable." Here’s what happens next:- Stop the infusion. No exceptions.
- Position you flat with legs raised to help blood flow to your heart and brain.
- Check vitals: Blood pressure, heart rate, oxygen levels.
- Give emergency meds based on severity:
- Grade 1-2 (mild to moderate): Diphenhydramine 50 mg IV, methylprednisolone 125 mg IV. Slow the infusion down, then restart at half speed after symptoms clear.
- Grade 3 (severe): Same meds, plus adrenaline 0.3-0.5 mg IM in the outer thigh. Repeat every 5 minutes if needed. Oxygen, IV fluids, and close monitoring.
- Grade 4 (life-threatening): Adrenaline immediately. Intubation if breathing fails. Never restart the biologic after a Grade 4 reaction. Studies show 22% of patients who try again have another life-threatening event.
Desensitization: Getting Back on Track After a Reaction
If you had a reaction but your doctor says the drug is still your best option, desensitization is your path forward. It’s not magic-it’s controlled exposure. The 12-step, 3-bag protocol is the most proven method:- Start at 0.1 mL/min with a tiny diluted dose.
- Gradually increase the dose over 4-6 hours.
- Each step is 10x the previous, with 15-30 minute waits in between.
- Final step: full dose at 5 mL/min.
What’s New in 2025?
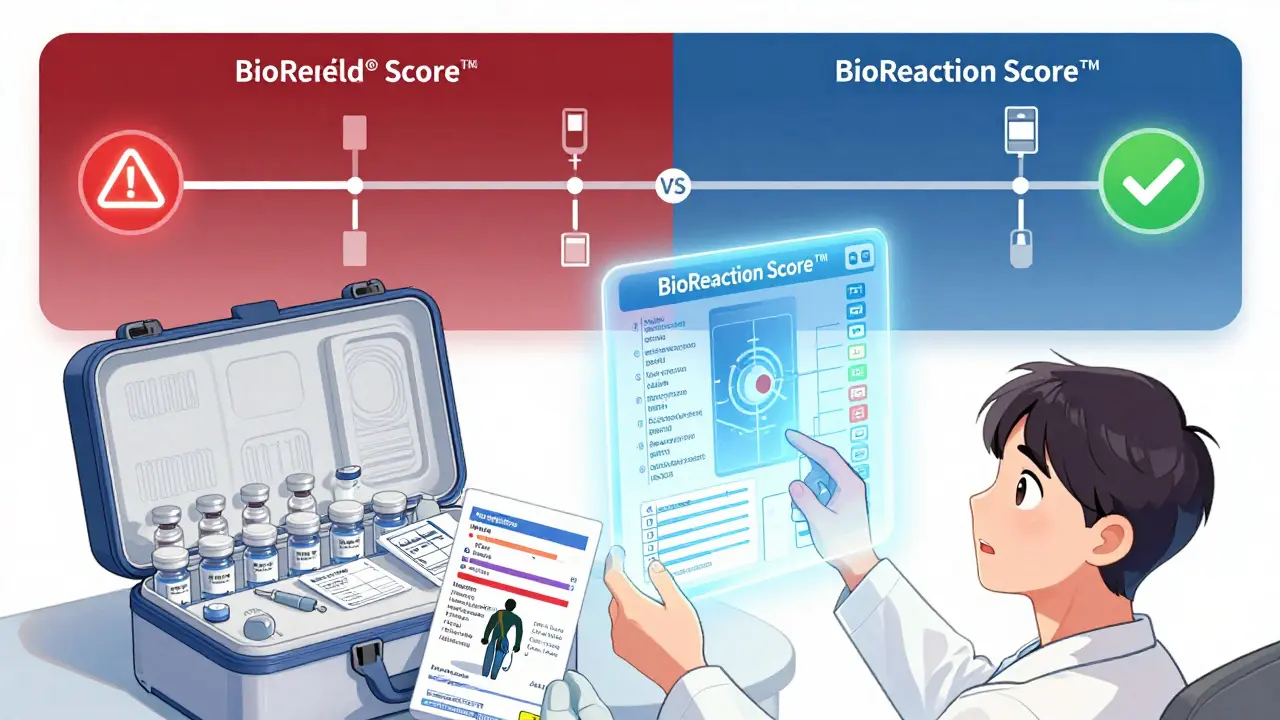
The field is moving fast. In 2024, the FDA approved the first standardized desensitization kit: BioShield®. It comes with pre-measured dilutions and printed protocol cards for 12 common biologics. No more manual calculations. No more errors. The NIH’s DESERVE trial is testing a faster 8-step protocol with real-time IL-6 monitoring. Early results? 98.2% success rate. That’s huge. And now there’s BioReaction Score™, an AI tool that predicts your risk of a reaction with 87.4% accuracy. It looks at your IL-6 levels, your HLA-DRA*0102 gene status, and even past antibiotic reactions. If you’re due for a biologic, ask if your clinic uses this.What You Need to Know Before Your Next Infusion
You’re not powerless. Here’s your checklist:- Confirm you’re getting premeds: steroid, antihistamine, acetaminophen.
- Ask if they’re using a hydration protocol.
- Make sure the infusion starts slow-no rushing.
- Know your symptoms: if you feel odd, speak up.
- Ask if they’ll check your serum tryptase 60 minutes after any reaction. Levels above 11.4 µg/L plus 20% of your baseline confirm anaphylaxis.
- If you’ve had a reaction before, ask about desensitization.
Why This Matters
Biologics are now the backbone of treatment for millions. The global market hit $387 billion in 2024-and it’s growing. But without proper reaction management, patients drop out. And that’s not just a number. It’s someone losing their chance at remission. The data is clear: protocols work. Desensitization saves treatments. Premedication reduces risk. Monitoring catches problems early. This isn’t theoretical. It’s happening in clinics every day. You don’t have to fear your infusion. You just need to know what to expect-and how to make sure your care team is ready.Can biologic infusion reactions be prevented completely?
No, they can’t be prevented 100% of the time, but the risk can be reduced by 70-80% with proper premedication, slow infusion rates, and hydration. Up to 40% of patients still experience mild reactions, but with protocols in place, most are manageable and don’t require stopping treatment.
How long does a desensitization protocol take?
A full 12-step IV desensitization takes 4 to 6 hours. Subcutaneous protocols take 3-4 hours. The process is slow by design-each step gives your immune system time to adjust. Patients often go home the same day after monitoring for 1-2 hours post-infusion.
Is it safe to get biologics again after a severe reaction?
Never restart a biologic after a Grade 4 (life-threatening) reaction. For Grade 3 reactions, desensitization under strict supervision is possible and successful in over 90% of cases. But only if the reaction wasn’t anaphylactic or caused organ failure. Always consult your specialist.
Do all biologics cause the same kind of reactions?
No. TNF inhibitors like infliximab cause more immediate hypersensitivity. Rituximab and trastuzumab are more likely to cause cytokine release syndrome, especially on the first infusion. Cetuximab uniquely triggers IgE-mediated reactions in people with pre-existing antibodies to alpha-gal, a sugar found in some meats. Each drug has its own risk profile.
Why do some clinics skip premedication?
Some clinics skip premeds to save time or due to lack of training. But studies show that without steroids and antihistamines, reaction rates double. The 2023 American College of Rheumatology survey found only 42% of clinics follow standardized protocols. If your clinic doesn’t use them, ask why-and consider seeking care elsewhere.
Can I take oral steroids instead of IV for premedication?
Oral steroids aren’t reliable enough for premedication. Absorption is slow and inconsistent. IV hydrocortisone or methylprednisolone ensures the drug hits your bloodstream fast and at the right level. Oral prednisone is not a substitute. If you’re given oral steroids before your infusion, ask if it’s part of a research protocol or if there’s a mistake.
What should I bring to my infusion appointment?
Bring your medication list, a list of past reactions (even mild ones), and a friend or family member to help you remember what happened. Wear comfortable clothes. Avoid eating a heavy meal right before-you might feel nauseous. If you’ve had reactions before, ask if you can have a copy of your desensitization protocol to keep on file.

Usha Sundar
December 23, 2025 AT 11:36Wilton Holliday
December 25, 2025 AT 05:51Harsh Khandelwal
December 26, 2025 AT 00:38Delilah Rose
December 27, 2025 AT 20:04Spencer Garcia
December 29, 2025 AT 11:24Bret Freeman
December 31, 2025 AT 09:34John Pearce CP
January 1, 2026 AT 02:40Ajay Sangani
January 1, 2026 AT 22:41Lu Jelonek
January 3, 2026 AT 08:06