Parkinson’s Disease and Antipsychotics: How Certain Medications Worsen Motor Symptoms

Parkinson's Antipsychotic Risk Checker
Medication Risk Assessment Tool
Select an antipsychotic to see its impact on Parkinson's motor symptoms. Based on research from the Parkinson's Foundation and peer-reviewed studies.
Quetiapine
Dopamine D2 Receptor Blockage: 5-10%
Motor Symptom Risk: Low
Effectiveness for Psychosis: Moderate (varies by study)
When someone with Parkinson’s disease starts seeing things that aren’t there-people in the room, shadows moving, or loved ones saying things they never said-it’s terrifying. Not just for the patient, but for everyone around them. This is Parkinson’s disease psychosis (PDP), and it affects about 24% of people with Parkinson’s, according to the Parkinson’s Foundation. The natural response is to reach for an antipsychotic. But here’s the cruel twist: the very drugs meant to calm the mind can slam the brakes on the body.
Why Antipsychotics Make Parkinson’s Worse
Parkinson’s is caused by the slow death of dopamine-producing neurons in the brain. Dopamine isn’t just about mood-it’s the fuel for smooth, controlled movement. Without it, you get tremors, stiffness, slow motion, and trouble balancing. That’s the motor side. The psychosis side? That’s thought to come from imbalances in other brain chemicals, especially serotonin and dopamine in different circuits. Most antipsychotics work by blocking dopamine receptors, especially the D2 type. That’s how they reduce hallucinations and delusions in schizophrenia. But in Parkinson’s, dopamine is already dangerously low. Blocking even more of it is like turning off the last few drops of fuel in an engine that’s already sputtering. The result? Motor symptoms get dramatically worse. Bradykinesia slows further. Rigidity tightens. Falls become more common. Some patients go from walking with a cane to needing a wheelchair in weeks. This isn’t theoretical. In the 1970s, doctors started noticing it. By 1996, the American Academy of Neurology formally warned about it. Today, we know the science behind it: drugs with high D2 receptor affinity are the worst offenders.The Worst Offenders: First-Generation Antipsychotics
First-generation antipsychotics (FGAs) like haloperidol, fluphenazine, and chlorpromazine are the most dangerous. Haloperidol (Haldol) is the poster child for this problem. At standard doses, it blocks 90-100% of D2 receptors. In Parkinson’s patients, even tiny doses-0.25 mg daily-can trigger severe parkinsonism. Studies show 70-80% of patients on haloperidol experience major motor decline. The Parkinson’s Foundation says FGAs should be avoided entirely. Not just avoided-forbidden. A 2005 double-blind trial in Movement Disorders compared risperidone (a second-generation drug) to clozapine. Risperidone reduced psychosis just as well as clozapine-but motor symptoms worsened by an average of 7.2 points on the UPDRS scale. Clozapine? Only 1.8 points. That’s a 4x difference in motor damage. And here’s the kicker: risperidone was linked to a 2.5 times higher risk of death in Parkinson’s patients, according to a 2013 Canadian study in JAMA Internal Medicine. Even olanzapine, once thought to be safer, caused motor worsening in 75% of patients in a 1999 study. Only one out of twelve stayed on it. Most had to be switched out.The Safer Options: Clozapine and Quetiapine
Not all antipsychotics are created equal. Two have earned a place in Parkinson’s care: clozapine and quetiapine. Clozapine is the gold standard. It blocks D2 receptors at only 40-60% occupancy-much lower than haloperidol. It also hits serotonin receptors, which helps stabilize mood without crushing movement. Since 2016, the FDA has approved it specifically for Parkinson’s psychosis. It works. In clinical trials, it cuts hallucinations by nearly half without worsening motor scores. But it’s not simple. Clozapine can cause agranulocytosis-a dangerous drop in white blood cells. That’s why patients need weekly blood tests. If neutrophils fall below 1,500 cells/μL, the drug must stop immediately. The risk is low-about 0.8%-but the monitoring is non-negotiable. Quetiapine (Seroquel) is used off-label. It’s easier to manage than clozapine. No blood tests. Lower risk. But here’s the controversy: some studies say it works. Others say it’s no better than a placebo. A 2017 trial by Factor et al. found no significant difference between quetiapine and sugar pills in reducing psychosis. Yet many neurologists still use it because it’s gentle on movement and works for some patients. It’s not a miracle, but it’s often the first try.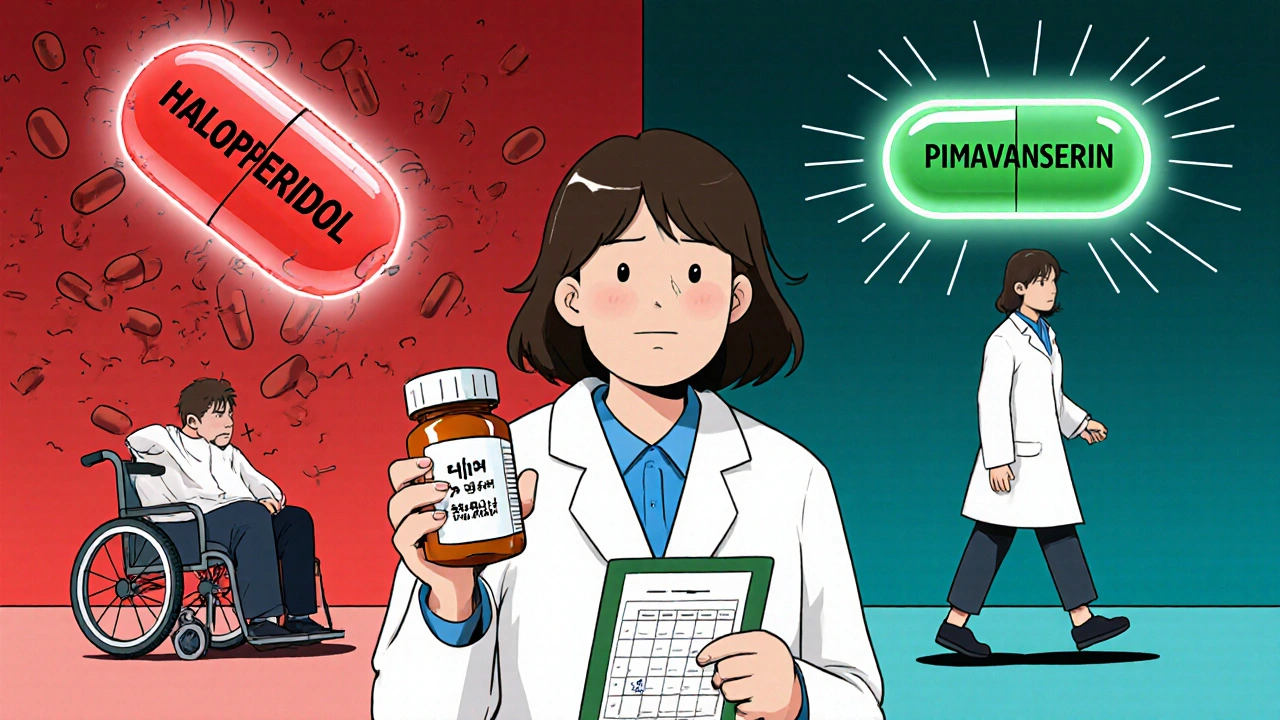
Pimavanserin: The First Non-Dopaminergic Option
In April 2022, the FDA approved pimavanserin (Nuplazid)-the first antipsychotic for Parkinson’s that doesn’t touch dopamine at all. It works by blocking serotonin 5-HT2A receptors, the same target as some migraine drugs. In the 2014-2018 trial, patients on pimavanserin saw a 5.79-point improvement in hallucinations with almost no motor worsening. That’s huge. But there’s a catch. Post-marketing data showed a 1.7 times higher risk of death compared to placebo. The FDA slapped on a black box warning. It’s still used, but only after other options fail-and only when the patient’s psychiatric symptoms are severe enough to outweigh the risk.The Real Solution: Don’t Use Antipsychotics Unless You Have To
The best treatment for Parkinson’s psychosis? Often, no antipsychotic at all. Before reaching for a pill to calm the mind, doctors should look at the meds that are already being taken. Many psychosis triggers are hidden in the Parkinson’s drug regimen. Anticholinergics like trihexyphenidyl? Cut them. Dopamine agonists like pramipexole or ropinirole? Reduce the dose. MAO-B inhibitors? Sometimes they contribute. Even levodopa can cause hallucinations at high doses. A 2018 study found that 62% of Parkinson’s patients with psychosis saw their symptoms disappear after simply adjusting their Parkinson’s meds-no antipsychotic needed. That’s more than half. The key is patience. It takes weeks to taper one drug and see the effect. But if you can avoid an antipsychotic entirely, you avoid the risk of falling, freezing, or becoming wheelchair-bound.
What to Do If You Need an Antipsychotic
If you’ve tried everything else and psychosis is still out of control, here’s the step-by-step:- Start with clozapine at 6.25-12.5 mg at night. Increase slowly over 4-6 weeks. Monitor blood counts weekly.
- If clozapine isn’t available or too risky, try quetiapine at 12.5-25 mg at night. Increase by 12.5 mg every 3-5 days, up to 100 mg daily if needed.
- Measure motor symptoms before and every two weeks using the UPDRS-III scale. If scores rise more than 30%, stop the drug.
- Never use haloperidol, risperidone, olanzapine, or any first-gen antipsychotic. Ever.
The Future: Lumateperone and Beyond
New drugs are on the horizon. Lumateperone (Caplyta), originally for schizophrenia, is now in phase III trials for Parkinson’s psychosis. Early results from the HARMONY trial show a 3.4-point improvement in hallucinations with no motor decline. Final results are expected in mid-2024. If it pans out, it could become the next safe option. The bigger picture? We’re moving away from dopamine-blocking drugs entirely. The goal isn’t just to treat psychosis-it’s to treat it without breaking the patient’s ability to walk, talk, or live independently.Bottom Line: Protect Movement First
Parkinson’s is already hard enough. The last thing you want is a medication that steals your mobility to fix your mind. Psychosis is real. It’s frightening. But it’s not always a medical emergency. Often, it’s a sign that something else in the treatment plan needs adjusting. If you or someone you care for has Parkinson’s and is experiencing hallucinations, talk to a neurologist who specializes in movement disorders. Don’t let a psychiatrist prescribe an antipsychotic without checking with the Parkinson’s team. The stakes are too high. One wrong pill can turn a person who walks into someone who can’t stand. The goal isn’t to eliminate every hallucination. It’s to keep the person safe, calm, and mobile. Sometimes, that means living with a few strange visions-rather than losing the ability to hold your grandchild’s hand.Can antipsychotics cause Parkinson’s symptoms in people who don’t have it?
Yes. Drugs that block dopamine, especially first-generation antipsychotics like haloperidol, can trigger drug-induced parkinsonism in people without Parkinson’s disease. This includes tremors, stiffness, and slow movement. It’s often reversible when the drug is stopped, but in some cases, symptoms persist for months or even years.
Is quetiapine safe for Parkinson’s patients?
Quetiapine is generally considered safer than other antipsychotics for Parkinson’s patients because it has low D2 receptor affinity and doesn’t significantly worsen motor symptoms in most people. But its effectiveness for psychosis is debated. Some studies show it works; others show no difference from placebo. It’s often used as a first-line option when clozapine isn’t available, but it’s not a guaranteed solution.
Why is clozapine not used more often if it’s the most effective?
Clozapine is the most effective antipsychotic for Parkinson’s psychosis, but it carries a small but serious risk of agranulocytosis-a life-threatening drop in white blood cells. That requires weekly blood tests for the first 6 months, then biweekly. Many patients and doctors avoid it because of the monitoring burden, even though the risk is low (0.8%). It’s reserved for cases where other treatments have failed.
Can reducing levodopa help with psychosis in Parkinson’s?
Yes. High doses of levodopa are a common trigger for hallucinations and delusions in Parkinson’s patients. Reducing the dose, splitting it into smaller amounts, or switching to a controlled-release form can significantly improve psychotic symptoms without worsening movement. In fact, up to 62% of patients see their psychosis resolve just by adjusting their Parkinson’s medications.
What should I do if a doctor prescribes haloperidol for my Parkinson’s psychosis?
Do not take it. Haloperidol can cause rapid, severe worsening of motor symptoms-even at very low doses. Ask for a second opinion from a movement disorder specialist. If the doctor insists, request documentation of why they’re choosing a drug with an 80-90% risk of making Parkinson’s worse. There are safer alternatives. Haloperidol should never be first-line, and in most cases, it should be avoided entirely.

Willie Doherty
November 21, 2025 AT 13:56The pharmacological paradox in Parkinson’s psychosis is well-documented, yet clinically underappreciated. The D2 receptor blockade mechanism, while efficacious in schizophrenia, is catastrophically misaligned with the dopaminergic deficit in Parkinson’s disease. The data from Movement Disorders (2005) and JAMA Internal Medicine (2013) are unequivocal: risperidone’s 7.2-point UPDRS deterioration and 2.5x mortality risk render it ethically indefensible in this population. Clozapine remains the only evidence-based antipsychotic with acceptable motor safety, despite its hematological monitoring burden. The 62% remission rate via dopaminergic regimen optimization underscores that psychosis is often iatrogenic-not primary. This is not neurology-it’s pharmacological triage.
Darragh McNulty
November 22, 2025 AT 14:49OMG this is so important!! 🙏 I’ve seen my uncle go from walking the dog to needing a wheelchair after they gave him Haldol. No one told us it could do THAT. Please, if you’re reading this and your doc wants to prescribe an antipsychotic-ask if it’s clozapine or quetiapine. If they say anything else, run. 💪❤️
David Cusack
November 24, 2025 AT 14:30One must question the clinical acumen of those who persist in prescribing FGAs-haloperidol, in particular-is not merely inappropriate, it is an affront to evidence-based medicine. The literature, spanning decades, is unequivocal. To prescribe such agents is not negligence-it is malpractice. The FDA’s black box warnings, the AAN guidelines, the UPDRS data-all ignored. One wonders whether such decisions stem from ignorance, inertia, or worse, institutional complacency. The consequences are not abstract-they are wheelchair-bound elders, fractured hips, and families shattered by preventable decline.
Elaina Cronin
November 24, 2025 AT 21:01I am deeply disturbed by the casual dismissal of patient safety in many psychiatric consultations. The notion that a patient with Parkinson’s should be subjected to haloperidol-despite overwhelming evidence of its catastrophic motor effects-is unconscionable. As a caregiver, I have witnessed the slow erosion of dignity that follows such prescriptions. No amount of reduced hallucinations justifies the loss of autonomy, of mobility, of the ability to hold a grandchild’s hand. This is not treatment. This is chemical restraint disguised as care. I demand better.
Mark Kahn
November 26, 2025 AT 20:53This is such a helpful breakdown-thank you for writing this! I’m a nurse in a neuro clinic and we’ve had so many patients come in after their psych doc prescribed risperidone. We always have to undo the damage. The part about adjusting levodopa first? Game changer. We’ve had three people stop hallucinating after just lowering their nighttime dose. No antipsychotic needed. Seriously, if you’re dealing with this, talk to a movement disorder specialist before signing anything. You’ve got this!
Daisy L
November 27, 2025 AT 18:12So let me get this straight-we have a drug (pimavanserin) that doesn’t even touch dopamine, works better than half the crap they used to shove down people’s throats, and the FDA still slaps a BLACK BOX on it because some old folks died? Meanwhile, haloperidol? Still floating around like a ghost in the machine. This isn’t medicine-it’s a bureaucratic horror show. They’d rather risk death than admit they need to update their protocols. And don’t even get me started on insurance refusing clozapine because ‘it’s too expensive to monitor.’ Bullshit. We monitor chemo. We monitor TB. We monitor pregnancy. But a man who can’t walk? Nah. Let him fall.
Corra Hathaway
November 29, 2025 AT 10:42Y’all. I just got off the phone with my mom’s neurologist. She’s been on quetiapine for 6 months and her hallucinations? Gone. And she’s still dancing at family weddings! 🎉💃 I know some studies say it’s placebo-but if it works, it works. And if it keeps your grandma from getting stuck in a wheelchair? Sign me up. Also-DO NOT let anyone give you haloperidol. I repeat: DO NOT. I’ve seen what it does. It’s like turning off the lights in a house that’s already on fire. 🚫💊
Paula Jane Butterfield
December 1, 2025 AT 06:15Hey everyone-just wanted to share my dad’s story. He had PDP and they tried everything. Risperidone made him freeze up. Olanzapine gave him drooling fits. Then they switched to clozapine. First week, he could barely walk. But by week 5? He was gardening again. The blood tests were a pain-weekly pokes, so much paperwork-but it was worth it. He’s been on it for 3 years now. No falls. No wheelchair. And he still tells me about the lady in the kitchen who brings him tea every morning… but now he knows she’s not real. That’s the win. It’s not about erasing the visions-it’s about keeping him safe. And if you’re scared of clozapine? Talk to a movement disorder specialist. They’re the real MVPs. (Sorry for typos-typing with one hand while holding my coffee! ☕)
Simone Wood
December 1, 2025 AT 10:53Look-I’m not a doctor but my sister’s husband was on Haldol for 3 weeks and suddenly couldn’t lift his spoon. The psych ward said ‘it’s just side effects’ and kept giving it to him. The neurologist finally said ‘stop it’ and he got better. But now he has permanent tremors. This isn’t science. This is a systemic failure. And don’t even get me started on how insurance won’t cover clozapine unless you’re ‘end-stage.’ End-stage of what? Of being able to feed yourself? This is a moral crisis. And no one’s talking about it. #ParkinsonsCrisis