Cost vs Benefit: When Expensive Medications Make Sense Despite Side Effects
Drug Cost-Benefit Calculator
Value Assessment Tool
Enter your specific situation to see if an expensive medication might be worth it. This tool compares cost against survival benefits and quality of life improvements.
Your Results
Value per QALY:
How This Compares:
Key Note: This tool uses clinical benchmarks to show if a treatment is likely to be considered cost-effective. The UK's NICE threshold is £30,000 per QALY. In the U.S., there's no official standard, but many insurers use similar benchmarks.
Is This Worth It?
When a drug costs more than your annual rent, and the side effects leave you exhausted, nauseated, or worse - why would anyone take it? The answer isn’t simple. For some people, these medications aren’t just an option - they’re the only thing standing between them and a life of pain, disability, or early death. The real question isn’t whether the drug is expensive. It’s whether it’s worth it.
Why Some Drugs Cost More Than a Car
You’ve probably heard the headlines: a single dose of a new cancer drug costs $50,000. A gene therapy for a rare blood disorder runs $3 million. These numbers feel absurd. And they are - but not because the science is flawed. They’re high because the development process is broken. Most new drugs aren’t revolutionary. A 2023 analysis found only 7 out of 100 newly approved medications offered real progress over what already existed. Yet companies charge like they’re the first to invent insulin. The real cost drivers? Rare diseases. Cancer. Autoimmune conditions. These are the areas where drugmakers focus because they can. The Orphan Drug Act of 1983 gave companies tax breaks and market exclusivity for treatments targeting fewer than 200,000 patients in the U.S. That’s why 72% of the 50 most expensive drugs in 2024 were for rare conditions. They don’t need mass sales to turn a profit. One patient paying $400,000 a year can fund an entire R&D department.Side Effects Aren’t the Problem - Lack of Alternatives Is
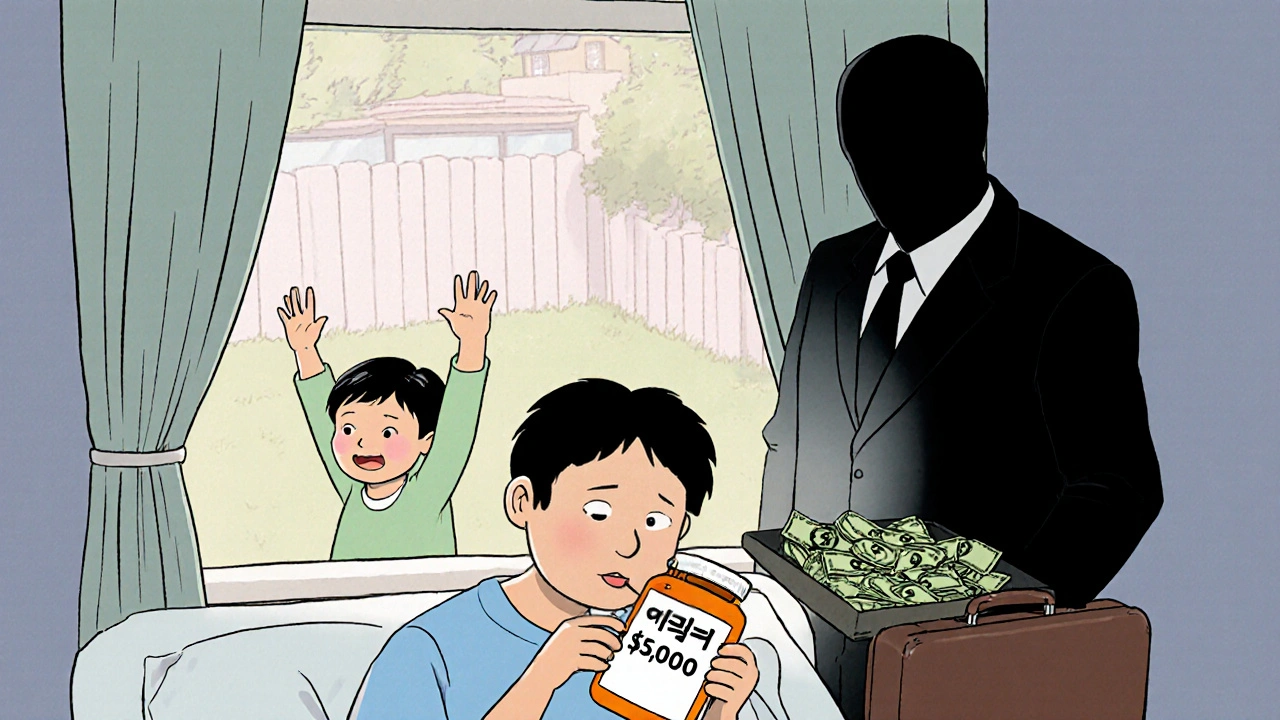
Let’s talk about side effects. Yes, some of these drugs cause severe reactions. CAR-T cell therapy for leukemia can trigger cytokine release syndrome - a dangerous immune storm that requires ICU care. Hepatitis C drugs like Harvoni might cause headaches and fatigue. But compare that to what came before. Older hepatitis treatments required weekly injections, caused flu-like symptoms so bad patients couldn’t work, and only worked half the time. Harvoni cured 95% of patients in 12 weeks. The side effects? Mild. The cost? $7,000 out-of-pocket in 2016. For many, that was a fair trade. The same goes for hemophilia. Emicizumab, a monthly injection that costs $15,000 a month, replaced daily infusions that often failed, leading to joint destruction and chronic pain. One Reddit user wrote: “I was in a wheelchair at 28. Now I walk my dog every morning. The cost? I’m still paying. But I’m alive.” Side effects matter. But when the alternative is a slow, painful decline, the math changes.What Does ‘Value’ Really Mean?
In the U.S., there’s no official rule for what’s “worth it.” In the UK, the National Institute for Health and Care Excellence (NICE) says a treatment should cost no more than £30,000 per extra year of healthy life - called a QALY. If a drug costs £120,000 per QALY, it gets rejected. Daratumumab, a multiple myeloma drug, was turned down in 2016 - until the manufacturer dropped the price. Then it was approved. In the U.S., no such rule exists. That means insurers, hospitals, and patients are left guessing. A 2024 study found that 56% of the most expensive drugs were rated as having low or no added benefit by health agencies in France and Germany. Yet they’re still prescribed here because, for some patients, there’s nothing else. The DrugAbacus tool, created by Dr. Peter Bach, measures drug value across six factors: survival gain, quality of life, side effects, innovation, cost, and patient burden. Of the top 10 cancer drugs approved in 2018, four didn’t meet the bar. But patients still took them. Why? Because for them, even a few extra months mattered.
Who Pays - And Who Suffers?
The real cost isn’t just in the pharmacy. It’s in the choices people make. A 2022 survey found 68% of patients on drugs costing over $10,000 a month skipped doses to save money. 42% chose between medicine and food. Medicare Part D beneficiaries without low-income help spent 2.5 times more out-of-pocket than those with private insurance. One patient on Revlimid, a multiple myeloma drug, paid $11,538 out-of-pocket in 2016 - 76% of that came after hitting the coverage gap, known as the “donut hole.” But here’s the twist: those who can afford it often get the best outcomes. A 2023 CMS report showed that 68% of low-income Medicare enrollees delayed or skipped doses. Only 22% of higher-income patients did. The system doesn’t just favor the wealthy - it forces the poor to gamble with their health.When It’s Worth It - Real Stories
There are moments when the cost doesn’t just make sense - it’s the only rational choice. Take tisagenlecleucel, a CAR-T therapy for pediatric leukemia. Each treatment costs $475,000. It requires hospitalization. Side effects include seizures and organ failure. But for kids who had run out of chemo options, it meant a 78% chance of long-term remission. In a 2023 patient forum, 78% of families said it was worth it - even if they had to sell their house. Or consider the hepatitis C cure. Before Harvoni, patients endured 48 weeks of injections, fever, depression, and a 50% cure rate. Now, a 12-week course cures 95% with mild fatigue. The upfront cost was brutal. But the long-term savings? No more liver transplants. No more dialysis. No more lost wages. The treatment paid for itself in three years.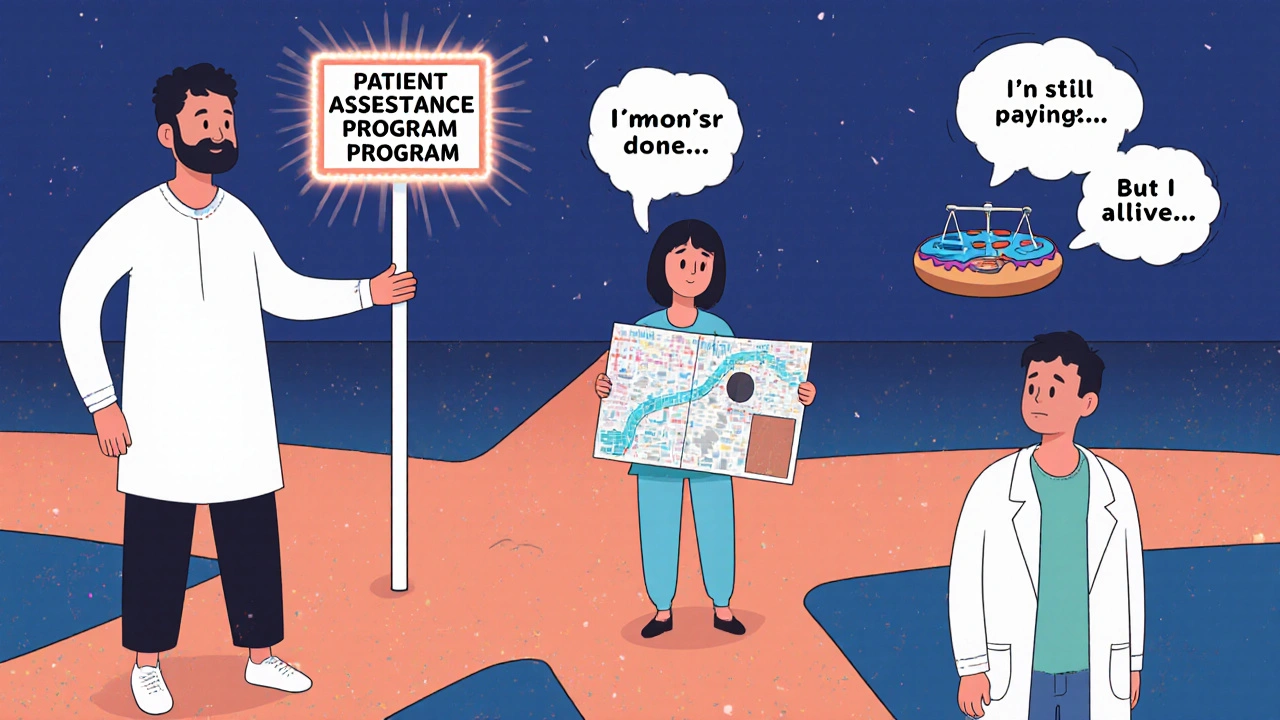
How to Navigate the System - If You Have To
If you’re facing a high-cost drug, you’re not alone. And you don’t have to pay full price.- Ask for manufacturer assistance. Most big pharma companies have patient support programs. On average, they cover 40% of out-of-pocket costs for commercially insured patients.
- Use independent foundations. The Chronic Disease Fund gave out $2.1 billion in aid in 2022. They help with co-pays for drugs like Humira, Enbrel, and Orencia.
- Work with a specialty pharmacy. These aren’t your local CVS. They assign case managers who spend over 3 hours per patient navigating insurance, prior authorizations, and appeals. It’s slow, but it works.
- Know your insurance phases. Medicare Part D has four stages: deductible, initial coverage, coverage gap (donut hole), and catastrophic. Once you hit catastrophic, your out-of-pocket drops to 5%. That’s when the real savings kick in - if you can survive until then.
- Ask for alternatives. Not every expensive drug is the only option. Sometimes a generic, an older biologic, or even a lower-dose version can work. Don’t assume the doctor’s first choice is the only one.
The Bigger Picture - Is This Sustainable?
The U.S. spent $621 billion on prescription drugs in 2022. Specialty drugs - the expensive ones - made up 54% of that spending, even though they account for only 3% of prescriptions. The orphan drug market is growing at 12% a year. By 2030, specialty drugs will make up 79% of all pharmacy spending. The Inflation Reduction Act of 2022 started a slow shift. For the first time, Medicare can negotiate prices on 10 high-cost drugs starting in 2026. But here’s the catch: 96% of the most expensive drugs are excluded because they’re too new, too rare, or too complex. The system is still tilted toward profit, not patient need. Meanwhile, Europe is moving toward joint assessments. By 2025, all new drugs in the EU will be evaluated by a centralized team. They’ll look at clinical benefit, side effects, and cost - together. The U.S. is still playing catch-up.Final Thought: It’s Not About the Price - It’s About the Choice
No one wakes up and says, “I hope my drug costs $50,000.” But when your body is failing, and every other option has failed too, the price tag becomes secondary. What matters is whether you can still hold your child’s hand. Walk to the mailbox. Sleep through the night. Expensive drugs aren’t the problem. The problem is a system that lets companies charge whatever they want - and leaves patients to decide between survival and bankruptcy. Until that changes, the only way to make sense of the cost is to look at the benefit - not in dollars, but in days.Are expensive medications always worth the side effects?
No. Many expensive drugs offer little to no real benefit over cheaper alternatives. Studies show that 56% of the top 50 most expensive drugs were rated as having low or no added therapeutic value by European health agencies. But for patients with no other options - like those with rare cancers or advanced autoimmune diseases - even a small improvement in survival or quality of life can make the side effects worth enduring.
Why are some drugs so much more expensive in the U.S. than in other countries?
The U.S. doesn’t negotiate drug prices or set cost-effectiveness limits like the UK or Germany. Drugmakers can charge whatever the market will bear. In Europe, agencies like NICE and IQWiG reject drugs that don’t offer enough benefit for the price. In the U.S., insurers often pay full list price because they have no leverage. That’s why a drug costing $10,000 in Canada can cost $50,000 in the U.S.
Can I get financial help for high-cost medications?
Yes. Most drug manufacturers offer patient assistance programs that cover 30-60% of out-of-pocket costs. Independent nonprofits like the Chronic Disease Fund and Patient Access Network Foundation have given over $2 billion in aid since 2020. Specialty pharmacies also assign case managers who help with insurance appeals and prior authorizations - often reducing costs by thousands per year.
What’s the difference between list price and net price?
The list price is what the drugmaker charges pharmacies - often inflated to make discounts look bigger. The net price is what the insurer actually pays after rebates and discounts. These rebates are secret, and patients rarely see the benefit. For example, a drug might have a $100,000 list price, but the net price after rebates could be $60,000. You still pay based on the list price, which is why your co-pay is so high.
Will Medicare negotiate prices for expensive drugs?
Starting in 2026, Medicare will negotiate prices for up to 10 drugs per year. But 96% of the most expensive drugs are currently excluded because they’re too new, too rare, or don’t meet the eligibility criteria. The law only targets drugs that have been on the market for at least nine years and have high Medicare spending. So while it’s a step forward, it won’t fix the problem for most patients today.
How do I know if a drug is truly innovative or just overpriced?
Check independent reviews from Prescrire International or the Institute for Clinical and Economic Review (ICER). They rate new drugs on clinical benefit, side effects, and comparison to existing treatments. Only about 15% of new drugs are rated as offering major therapeutic progress. If a drug claims to be a breakthrough but has no clear advantage over a $50 generic, it’s likely overpriced.

Nikhil Purohit
November 20, 2025 AT 14:53Man, I read this and thought about my cousin in Mumbai who’s on a $20k/month drug for rheumatoid arthritis. He takes it because he can’t hold his grandson otherwise. Side effects? He’s always tired. But he’s alive. And that’s the real math.
Debanjan Banerjee
November 22, 2025 AT 01:19The real issue isn’t drug pricing-it’s the absence of value-based reimbursement frameworks. The U.S. healthcare system incentivizes volume over outcomes, and pharmaceutical companies exploit this via patent evergreening and strategic market exclusivity under the Orphan Drug Act. ICER’s analyses consistently demonstrate that >50% of high-cost biologics offer marginal incremental benefit.
Michael Marrale
November 23, 2025 AT 20:32Ever wonder why Big Pharma is secretly funded by the Illuminati? They don’t want you to know that the real cure for cancer was invented in 1987 but buried because it’s a $5 herbal tea. These drugs? Total scam. They’re just keeping you dependent so you keep buying. Google ‘Project Monarch drug control’.
David vaughan
November 24, 2025 AT 06:49I just… I just want to say… I’m so glad someone finally wrote this. I’ve been on Humira for 7 years. My joints used to scream at night. Now? I can hug my wife without crying. The co-pay is $1,200/month… but I’d pay $12,000. I’m not rich. But I’m alive. And that’s… that’s enough.
Chris Vere
November 24, 2025 AT 23:09It is interesting how the concept of value is constructed in capitalist systems. The body becomes a ledger. Pain is quantified. Life is measured in QALYs. But what of dignity? What of the silent sacrifices of those who choose to live despite the cost? The system does not see them. It only sees the numbers.
Pravin Manani
November 26, 2025 AT 22:15Let’s talk about the pharmacoeconomic arbitrage here. When you have a drug with a marginal survival gain-say, 2.3 months-and a 40% incidence of grade 3+ toxicity, but no biosimilar competition due to patent thickets, the cost-per-QALY skyrockets. That’s not innovation. That’s regulatory capture disguised as R&D. The FDA’s accelerated approval pathway needs serious recalibration.
Mark Kahn
November 27, 2025 AT 09:57If you’re reading this and stressed about your meds-take a breath. You’re not alone. Talk to your pharmacist. Ask for the manufacturer’s patient assistance program. Most have sliding scales. Some give drugs for free. You don’t have to suffer in silence. You deserve to live. And there are people who want to help you get there.
Leo Tamisch
November 28, 2025 AT 03:05Wow. Such deep thoughts. 🤔 So profound. I mean, like… wow. The human condition, man. We’re all just atoms trying to survive in a matrix of capitalist dystopia. 🍕💊 But hey-did you know that the real reason these drugs cost so much is because the FDA is owned by Big Pharma? And also, the moon landing was faked. Just saying. 🌕
Simone Wood
November 29, 2025 AT 22:55OMG I JUST GOT DIAGNOSED WITH MULTIPLE MYELOMA AND THEY WANT ME TO TAKE REVLIMID FOR $12K A MONTH AND I’M 24 AND MY PARENTS ARE GOING BANKRUPT AND I JUST CRIED IN THE PHARMACY AND NOW I’M ON HERE CRYING AGAIN WHY IS LIFE LIKE THIS 😭😭😭
Swati Jain
December 1, 2025 AT 05:29Oh sweetie, you think $50k is bad? Try getting a $1.2M gene therapy approved when your insurance says ‘not medically necessary’ because you’re ‘too old’ to benefit. Meanwhile, the CEO of the company just bought a private island. 💅 The system is rigged. But hey-at least you’re getting ‘care.’
Florian Moser
December 2, 2025 AT 14:32One thing I’ve learned from working in oncology: the most expensive drugs aren’t always the best-but they’re often the only thing left. I’ve seen patients choose between paying for rent or their chemo. I’ve seen kids live longer because of a $400k treatment. It’s not fair. But it’s real. And we owe it to them to fight for better systems-not just accept the cost.
jim cerqua
December 3, 2025 AT 16:05Let me tell you about my sister. She took that CAR-T therapy. Seizures. ICU. Lost 30 pounds. Her hair fell out in clumps. She cried every night for a week. But she’s alive. And last week, she danced at her daughter’s wedding. No wheelchair. No IV pole. Just her. In heels. And I’ll tell you this: if that drug cost a million dollars? Worth it. A thousand times worth it. This system is broken-but the people? They’re warriors.
Erika Sta. Maria
December 3, 2025 AT 23:38Actually… you’re all wrong. The real problem is that people are too lazy to eat turmeric and do yoga. These drugs are a scam. The body heals itself if you just believe enough. Also, I read on a blog that the FDA is controlled by aliens who want us to stay sick so they can harvest our fear. My cousin’s aunt’s neighbor cured his cancer with lemon juice and a crystal. You’re all just brainwashed.
Steve Harris
December 4, 2025 AT 12:38Thank you for writing this. It’s rare to see the human side of this issue. I’ve worked in hospital pharmacy for 18 years. I’ve seen patients cry because they can’t afford their insulin. I’ve seen families sell cars. I’ve seen people skip doses to make it last. This isn’t healthcare. It’s a lottery. And the system needs to change-not just for the rich, but for everyone who’s still breathing.